Sharing meals with family and friends is one of the major highlights of the holiday season. Whether you treat yourself to old recipes or you try new ones, consider adding these eye-healthy foods to your holiday feast!
LEAFY GREEN VEGETABLES
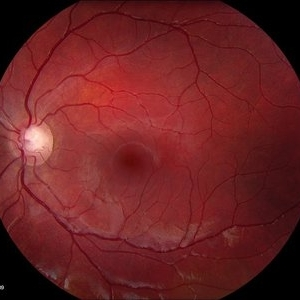
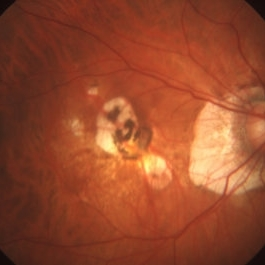
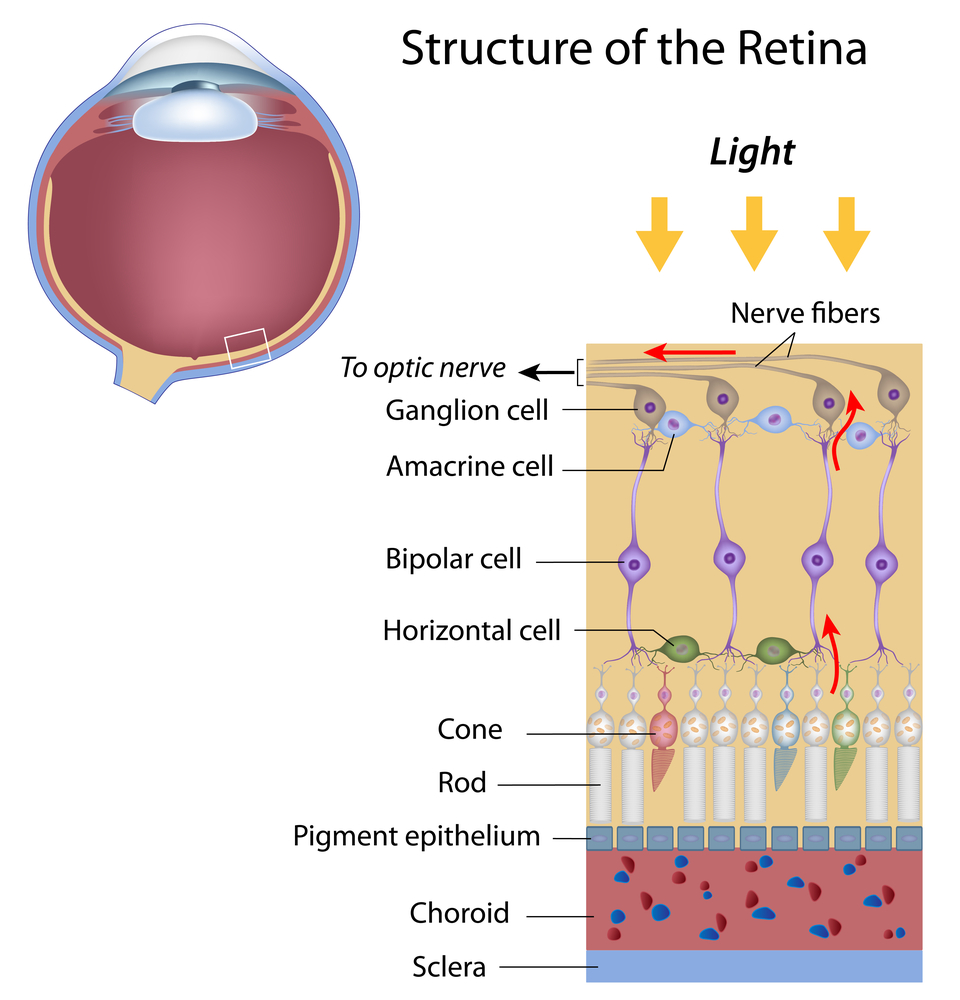
 Be sure to start your holiday meal with a salad, it’s an excellent way to ensure that you and your guests get plenty of zeaxanthin and lutein, two nutrients that help protect your central vision. Adding kale, spinach, or romaine lettuce to salads helps your eyes absorb damaging blue light, combats the effects of cigarette smoke and pollution, and also decreases your risk of developing age-related macular degeneration (AMD), a condition that affects the macula, the part of your retina responsible for central vision. You will also find lutein in grapes, kiwis, broccoli, peas, corn, Swiss chard, and collard greens.
Be sure to start your holiday meal with a salad, it’s an excellent way to ensure that you and your guests get plenty of zeaxanthin and lutein, two nutrients that help protect your central vision. Adding kale, spinach, or romaine lettuce to salads helps your eyes absorb damaging blue light, combats the effects of cigarette smoke and pollution, and also decreases your risk of developing age-related macular degeneration (AMD), a condition that affects the macula, the part of your retina responsible for central vision. You will also find lutein in grapes, kiwis, broccoli, peas, corn, Swiss chard, and collard greens.
TURKEY AND BEEF
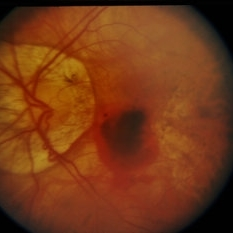
 Turkey and lean beef, two of the main ingredients in many holiday meals, keep your eyes strong and healthy. Both foods are high in zinc, a nutrient important to the retina and the choroid layer under the retina.
Turkey and lean beef, two of the main ingredients in many holiday meals, keep your eyes strong and healthy. Both foods are high in zinc, a nutrient important to the retina and the choroid layer under the retina.  Zinc is essential for good night vision. Eating foods that are high in the nutrient can also reduce your risk of cataracts and AMD. Other foods that contain zinc include pork, dairy products, chick peas, black-eyed peas, crab, oysters, beans, spinach, mushrooms, cashews, and almonds.
Zinc is essential for good night vision. Eating foods that are high in the nutrient can also reduce your risk of cataracts and AMD. Other foods that contain zinc include pork, dairy products, chick peas, black-eyed peas, crab, oysters, beans, spinach, mushrooms, cashews, and almonds.
CARROTS
 It wasn’t an old wives tale, it is true Carrots are good for your eyes! They contain beta carotene, a substance that turns into vitamin A when eaten. Eating carrots can benefit your night vision and could possibly reduce your risk of cataracts, AMD, and dry eyes. Other foods that contain beta carotene include pumpkin, sweet potatoes, and butternut squash. All great ingredients to include into your holiday feast.
It wasn’t an old wives tale, it is true Carrots are good for your eyes! They contain beta carotene, a substance that turns into vitamin A when eaten. Eating carrots can benefit your night vision and could possibly reduce your risk of cataracts, AMD, and dry eyes. Other foods that contain beta carotene include pumpkin, sweet potatoes, and butternut squash. All great ingredients to include into your holiday feast.
FISH
 Fish contain omega-3 fatty acids, which can reduce your risk of developing AMD, dry eye, and glaucoma. Salmon, mackerel, flounder, tuna, halibut, herring, and sardines would be a great addition to your holiday meals.
Fish contain omega-3 fatty acids, which can reduce your risk of developing AMD, dry eye, and glaucoma. Salmon, mackerel, flounder, tuna, halibut, herring, and sardines would be a great addition to your holiday meals.
WHOLE GRAINS
 Whole grains reduce your risk of heart disease, obesity, and type 2 diabetes and can also decrease your risk of AMD. Substituting whole grain flour for white flour in holiday breads and muffins is a simple way to boost your whole grain intake. Other good whole grain sources include wild rice, brown rice, popcorn, oatmeal, bulgur, barley, buckwheat, and couscous.
Whole grains reduce your risk of heart disease, obesity, and type 2 diabetes and can also decrease your risk of AMD. Substituting whole grain flour for white flour in holiday breads and muffins is a simple way to boost your whole grain intake. Other good whole grain sources include wild rice, brown rice, popcorn, oatmeal, bulgur, barley, buckwheat, and couscous.
FRUIT
 Fruits high in vitamin C, such as strawberries and oranges, also offer important vision benefits. Vitamin C is an antioxidant, a substance that can prevent cell damage caused by free radicals. Vitamin C-rich foods help keep the collagen in your cornea healthy and reduce the risk of cataracts and AMD. You can also find vitamin C in grapefruit, kiwi, blueberries, peas, broccoli, and tomatoes.
Fruits high in vitamin C, such as strawberries and oranges, also offer important vision benefits. Vitamin C is an antioxidant, a substance that can prevent cell damage caused by free radicals. Vitamin C-rich foods help keep the collagen in your cornea healthy and reduce the risk of cataracts and AMD. You can also find vitamin C in grapefruit, kiwi, blueberries, peas, broccoli, and tomatoes.
Sensible food choices, along with regular eye examinations, can help you protect your vision. For eye healthy recipes, visit our EYE COOK section in our website.
Happy Eating and Happy Holidays!