As you give thanks today, be thankful for being able to see. Here are some vision tips to keep your eyes healthy.
12 Thanksgiving Vision Tips
When you are giving thanks today, be sure to be thankful for your vision. In order to you keep your eyes healthy, here are 12 vision tips.
11/26/15
 Susan DeRemer, CFRE
Susan DeRemer, CFRE
Vice President of Development
Discovery Eye Foundation
#GivingTuesday – Giving For Eye Research
Medical research funding from the US government, the medical device and pharmaceutical industries, biotech and foundations has dropped 0.8% per year, every year from 2007 to 2012. Even with the economic recovery, the funding of eye research from the NIH in 2014 decreased by 17% from 2012.
What makes this particularly disturbing is that the need for eye research is more important now than ever, as demonstrated by the infographic below.
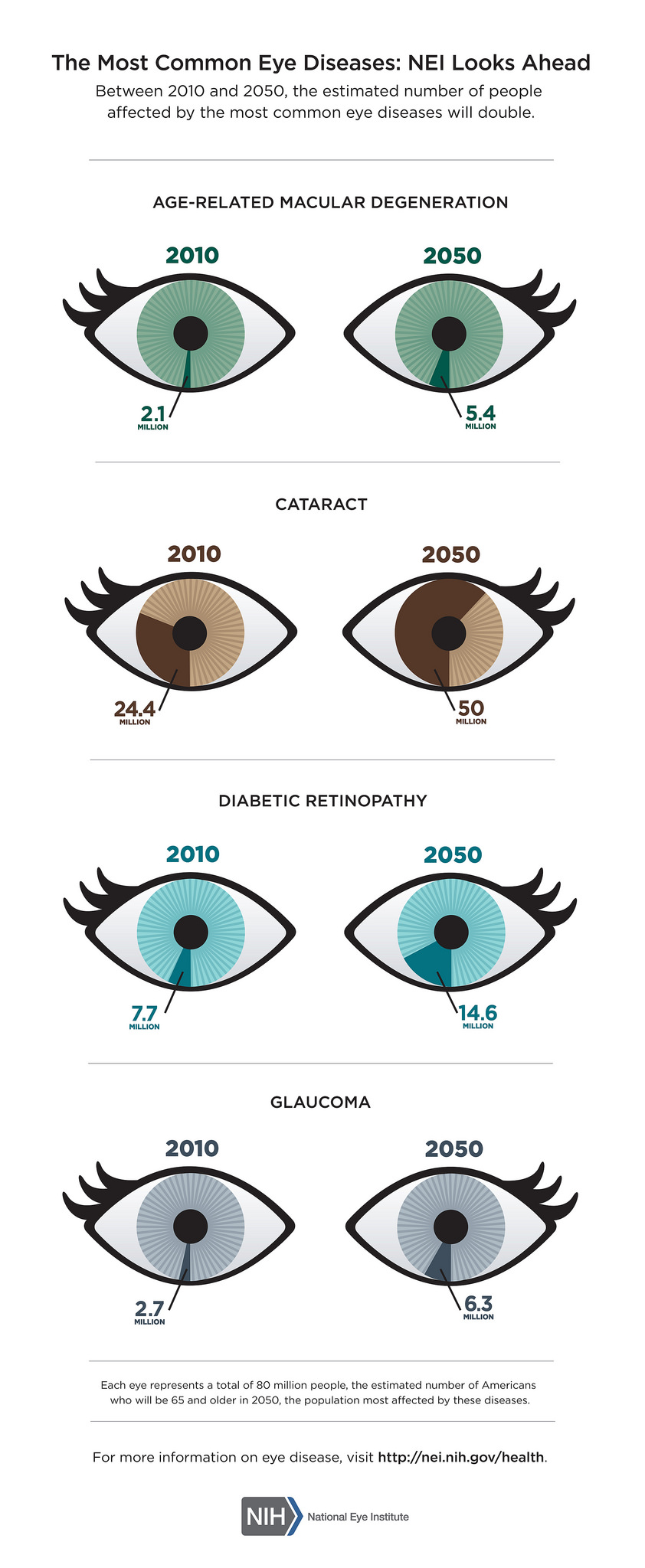
Giving For Eye Research
The eye diseases in the above graphic are related to aging. The number of people being affected is more than doubling for each eye diseases, except for diabetic retinopathy which will increase by 47%, by 2050.
While we are more health conscious than in previous years, knowing the importance of exercise, healthy eating and not smoking, the US population is aging.
Aging baby boomers, the largest population group in US history, are creating a dramatic shift in the age composition of the U.S. population. It is projected that the entire senior population, including the pre-boomer silent generation, will reach 71.4 million people by 2029. This means that those people 65 and older will make up about 20%of the US population by 2029, up from almost 14% in 2012.
We need your help to find treatments and cures for these sight-threatening eye diseases.
December 1st will be the fourth year of #GivingTuesday. It is a global day of giving using combined power of social media and collaboration. Always the Tuesday following Thanksgiving, it has become as widely recognized as Black Friday and Cyber Monday and kicks off the philanthropic season, when many focus on their holiday and end-of-year giving.
We are asking that you support eye research through the Discovery Eye Foundation this philanthropic season with a gift on #GivingTuesday. It is easy to do; you can do it from the comfort of your home – just click here.
Also share this post with family and friends so they can also give the gift of sight this holiday season.
Thank you for reading our blog and for your support.
11/24/15
 Susan DeRemer, CFRE
Susan DeRemer, CFRE
Vice President of Development
Discovery Eye Foundation
Smoking and Your Eyes
Smoking is the single largest preventable cause of eye disease.

On the third Thursday of November each year, smokers across the nation take part in the Great American Smokeout, sponsored by the American Cancer Society. This might be the ideal time for you to stop smoking and ACS has information and resources you may find helpful.
Here are some things you should know about smoking and your eyes.
- Smoking at any age, even in your teens or twenties, increases your future risk for vision loss.
- The more you smoke, the higher your risk for eye disease.
- If you quit smoking, your risk for these eye diseases decreases considerably.
- Smoking increases your risk for cardiovascular diseases that indirectly influence your eyes’ health.
- Women who smoke during pregnancy increase their chance for a premature birth and a potentially blinding eye disease called retinopathy of prematurity (ROP).
- A smoker is two times more likely to develop macular degeneration compared with a nonsmoker.
- Smoking double your chance of forming cataracts and the risk continues to increase the more you smoke.
- Smoking doubles your diabetes risk which can lead to the blinding eye disease, diabetic retinopathy.
- Smokers are more than twice as likely to be affected by dry eye syndrome as a non-smoker.
- Second-hand smoke also makes dry eye worse, especially for contact lens wearers and post-menopausal women.
- If you smoke you can have a three-fold increase in the risk of developing AMD compared with people who have never smoked.
- Smoking appears linked to the development of uveitis with smokers having more than twice the risk of non-smokers.
If you are looking to stop smoking you may also want to check out Smokefree.gov which provides free, accurate, evidence-based information and professional assistance to help support the immediate and long-term needs of people trying to quit smoking.
11/19/15
 Susan DeRemer, CFRE
Susan DeRemer, CFRE
Vice President of Development
Discovery Eye Foundation
Creating Cybrids to Study Age-Related Diseases
DEF Research Director Dr. M. Cristina Kenney’s research has shown that the mitochondrial DNA from different ethnic/racial populations may play a key role in determining that population’s resistance or susceptibility to disease (see previous article on 11/12/15 – Mitochondria and Age-Related Macular Degeneration). In order to study these effects, Kenney has developed the cybrid model using mitochondria from subjects of different ethnic/racial groups (Figure 1). The comparison of an individual’s mitochondria with that from other ethnic/racial groups (African, European, Asian or Ashkenazi Jewish) allows us to determine if their mitochondria determine that population’s susceptibility or resistance to disease and to response to drugs.
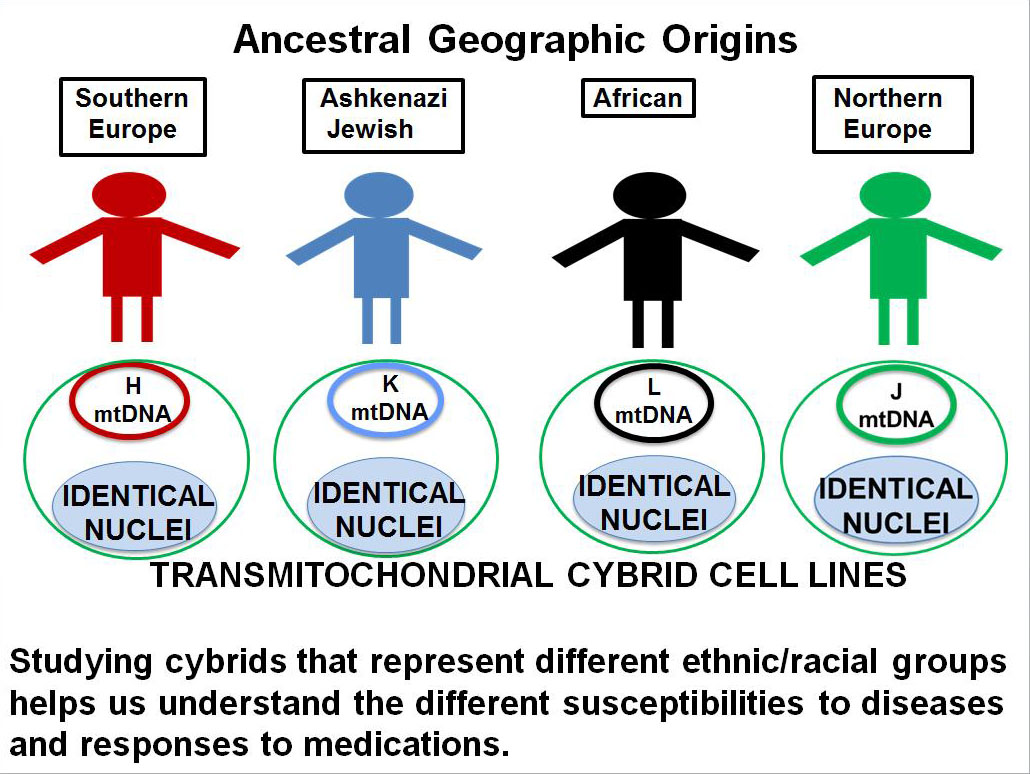
Personalized cybrids
Kenney’s cybrids are made with mitochondria from the blood taken from individual living donors. Looked at individually they are all really “personalized cybrids” because each cybrid test system has the mitochondria from the original donor and reflects the responses of that donor.
Using Cybrids to Study Age-Related Diseases
How is Kenney using these personalized cybrids?
Kenney is partnering with Dr. Pinchas Cohen, dean of the University of Southern California, Leonard Davis School of Gerontology, to explore how novel, small proteins produced from mitochondria might be used to treat a variety of age-related diseases such as age-related macular degeneration, Alzheimer’s, Parkinson’s, stroke and cholesterol. Cohen’s laboratory has discovered and characterized many of these new, small proteins called “mitochondrial derived peptides” (MDPs). His work has shown that these MDPs can protect brain cells from damage and early death, such as occurs in Alzheimer’s disease. Cohen and Kenney are now testing these MDPs in the K and H cybrids to assess their protective effects to stop retinal cell death, such as seen in AMD.
Kenney explains her approach:
“Our cybrid system represents a very powerful technique. We are now using the Ashkenazi Jewish population as an excellent model to learn how the mitochondria, with their unique mtDNA, influence the risk factors for AMD. We plan to extend the study to investigate Ashkenazi Jewish people’s susceptibility to Alzheimer’s disease, heart disease and stroke. Eventually, we believe the findings for the K haplogroup mitochondrial DNA will be applicable to other groups, as well.”
11/17/15
 Anthony B. Nesburn, MD, FASC
Anthony B. Nesburn, MD, FASC
President/Medical Director
Discovery Eye Foundation
Mitochondria and Age-Related Macular Degeneration
Research on mitochondrial DNA shows promise for treating AMD
For the past few years, DEF Research Director Dr. M. Cristina Kenney has been researching the relationship of mitochondria and age-related macular degeneration (AMD). She found that damaged mitochondria from people with AMD send signals that can cause retinal cells to die at an increased rate, compared with people who had healthy mitochondria and no AMD. That research led to the exploration of stimulating mitochondria to support retinal cell health in an effort to retain or restore vision for people with AMD.
Mitochondria in Cells
Cells are the basic building blocks of all living things. The human body is composed of trillions of cells. They provide structure for the body, take in nutrients from food, convert those nutrients into energy and carry out specialized functions. Cells also contain the body’s hereditary material (DNA) and so they can make copies of themselves.
Mitochondria are tiny structures inside cells whose function is to produce energy, like a battery in a flashlight, to keep cells alive. Each cell contains hundreds to thousands of mitochondria, which are located in the fluid that surrounds the nucleus. Although most DNA is packaged in chromosomes within the nucleus of a cell (nuclear DNA), mitochondria also have a small amount of their own DNA, known as mitochondrial DNA or mtDNA.
Because only egg cells contribute mitochondria to a developing embryo, only females can pass on the mitochondrial DNA to their children.
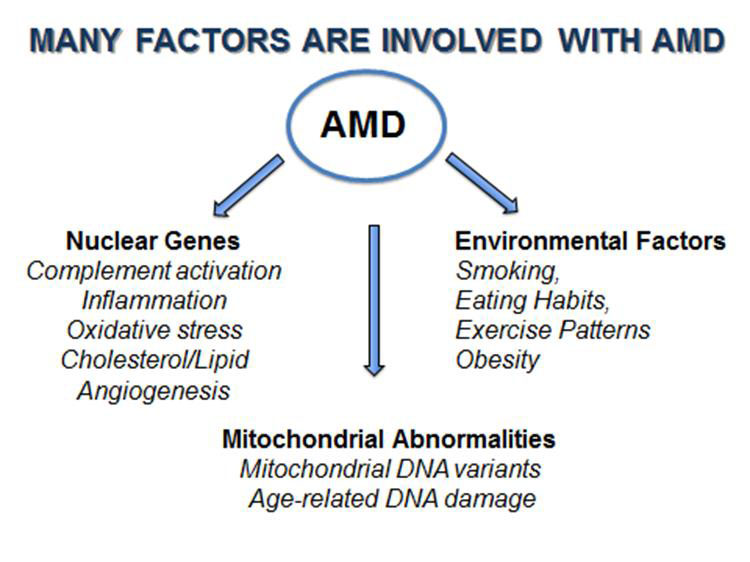
Mitochondrial Haplogroups
The mtDNA can be classified into categories called haplogroups, which represent different ancient, geographically separated groups of people. For example, African-Americans and people of ancient African lineage have inherited L haplogroup mitochondria from their mothers no matter where they currently live.
Similarly, most Ashkenazi Jewish populations (primarily those Jews whose families originated in Eastern or Central Europe) possess mitochondria of the K haplogroup. People with this haplogroup of mtDNA seem to be susceptible to a variety of age-related diseases, including age-related macular degeneration (AMD).
The incidence of AMD varies a lot among different ethnic/racial populations. For example, in the United States, the likelihood of losing vision from AMD is very low for a person with an African maternal background but it is much higher in people of European descent. Similarly, in an Israeli eye clinic, of the people who had AMD, 96% were Jewish while only 4% were of Arab descent. This suggests that European mtDNA in retinal cells of Caucasians may be the reason they are more susceptible to AMD.
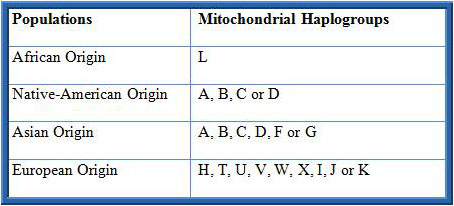
It has been recognized that AMD is a very complex disease with many factors involved (Figure 1). There are more than 30 genes associated with AMD, representing many different biological pathways. In addition, mitochondrial damage and specific mtDNA haplogroups have been associated with AMD. Finally, it is recognized that environmental factors, such as smoking and obesity, increase the risk to develop AMD.
Although millions of dollars and thousands of man-hours have been invested in finding the causes and treatments for AMD, we still do not understand how to prevent the most common form of AMD. One major difficulty has been that when we study a diverse group of individuals, each with hundreds of different nuclear and mitochondrial genes, it is very difficult to identify the causes and pathways involved with developing AMD and determining effective treatments. One drug may not help everyone and different people develop different types and severities of AMD.
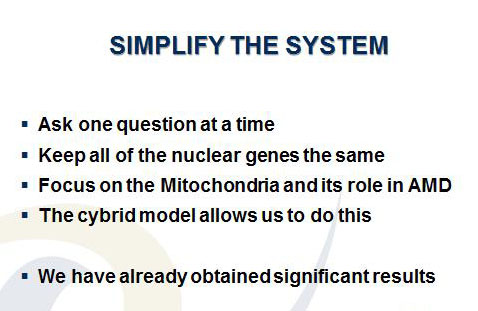
Kenney’s approach to this dilemma has been to SIMPLIFY THE TESTING SYSTEM (Figure 2). In her research with different ethnic/racial groups, Kenney has found that the Ashkenazi Jewish population (K haplogroup) is an excellent group in which to study age-related diseases. This group has very well characterized nuclear and mitochondrial genes, the population tends to relatively homogenous and to marry within their community. Finally, the Ashkenazi Jewish population has longevity, which increases the likelihood that they will develop aging diseases, such as AMD.
Kenney’s laboratory has created a “cybrid” test system, which are cell lines with identical nuclei and nuclear DNA, but different mitochondrial DNA so that the differences in the cell behavior can be attributed to the different mitochondrial DNA (see the following cybrid story on 11/17/15). Using the cybrid system, Kenney has compared cell behavior of mitochondria from subjects with the K (Ashkenazi Jewish) haplogroups and the mitochondria from people of the H haplogroup (Figure 3), the most common European haplogroup.
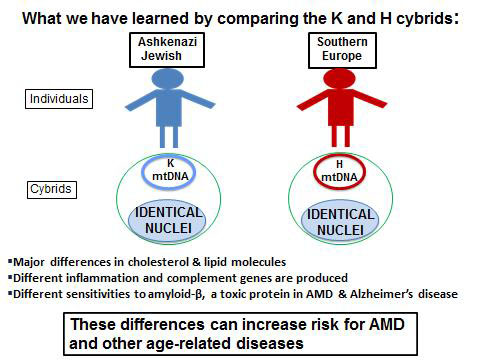
There are:
- Major differences in production of cholesterol and lipid molecules
- Altered levels of inflammation
- Differences in their responses to toxic effects of amyloid-? (a toxic protein associated with AMD and Alzheimer’s disease)
These differences are important contributors to AMD and other age-related diseases.
Significance of the Findings
Maternally inherited mitochondrial DNA can influence how a person’s cells respond to stress and this can contribute to age-related diseases. This is a completely new way of thinking about common aging diseases and offers new approaches to treatment and prevention of those diseases.
Future Studies
Kenney’s laboratory will continue to use the K haplogroup cybrid model to study the mitochondrial DNA, with the goal of blocking the harmful events that cause early retinal cell death, such as that seen in AMD. An additional advantage of cybrids is that they are unique to the donor whose blood was used to make them. Therefore with these “personalized cybrids,” Kenney can test the responses of the personalized cybrids to drugs that are currently being used for AMD (Lucentis™, Avastin™ and Eylea™). They can also be used to identify novel, new drugs that can protect the cells from early cellular death, a major event in the dry form of AMD. This research shows great promise in developing personalized treatments for AMD and other age-related diseases.
11/12/15
 Anthony B. Nesburn, MD FACS
Anthony B. Nesburn, MD FACS
President/Medical Director
Discovery Eye Foundation
Technology for Vision
In just over 10 years, the technology that has been developed to help people see has been amazing. While medical research continues to move forward to find treatments and potential cures of the future, those with the technological know-how have created ways for people to see NOW. Here is a very brief look at some of these technologies.
Technology for Vision
One of the pioneers in the field of vision technology, Second Sight started in 1998, and they are now currently producing the second version of their device. It is made up of two parts:
The Implant: Requiring a 4-hour surgery, a device is surgically implanted in the eye on top of the retina, and along the outside of the eye. It includes an antenna, an electronics case, and an electrode array.
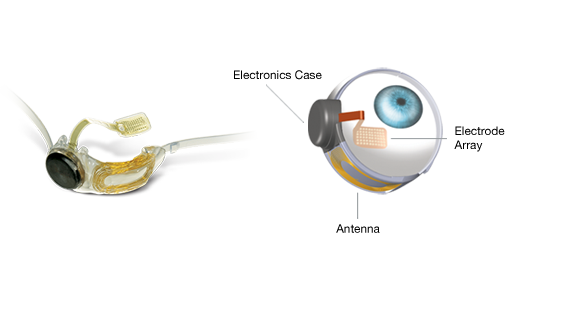
The External Equipment: It includes glasses, a video processing unit (VPU) and a cable.

In a healthy eye, photoreceptors (rods and cones) in the retina convert light into tiny electrochemical impulses that are sent to the brain, where they are translated into images. If the photoreceptors don’t function correctly your brain can’t produce images. The Argus II Retinal Prosthesis System (“Argus II”) is designed to bypass the damaged photoreceptors.
A miniature video camera housed in the patient’s glasses captures an object. The video is sent to the small VPU that the patient wears. It is then processed and transmitted back to the glasses via a cable. This information is sent wirelessly to the antenna in the implant and signals are sent to the electrode array, which emits small pulses of electricity. These pulses bypass the damaged photoreceptors and stimulate the retina’s remaining cells. The visual information is then sent to the brain to create the perception of patterns of light which patients can learn to interpret as objects. Significant training is required to use the system.
The implant is designed to give you a visual field of about 3.5 inches by 6.5 inches at arm’s length; however, the actual size of light you see may be larger or smaller. Since it is strictly based on light, there is no color perception.
Another system that relies upon the user wearing glasses is eSight which started in 2012. While the Argus II is for people that have very little or no vision, the eSight is for people with low vision or that are legally blind. eSight glasses require the individual to have a certain degree of sight remaining to be successful. If you can only see shadows you probably don’t have enough remaining sight for the glasses to work for them.
This system is also composed of two parts, but it does not require any surgery:
The Headset: It contains a high-definition camera, OLED screens, and the ability to capture and display a real-time video feed. The headset is mounted on carrier frames, which enables eSight’s “bioptic tilt” feature so the user can shift between viewing modes and engage their peripheral vision.
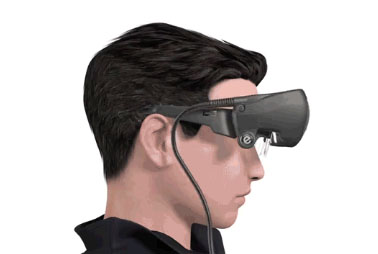
The Controller: A small, lightweight processing unit that adjusts every pixel of the video in real time. It also houses the battery, which powers eSight.
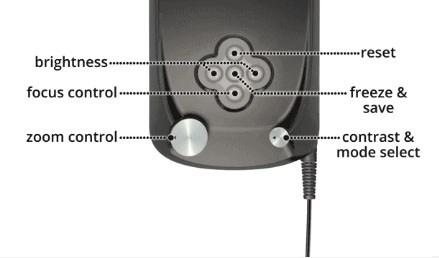
Because most legally blind individuals retain limited sight concentrated in their peripheral vision, their eyes do not receive an adequate signal for the brain to recognize what is being seen. This can create blind spots, blurriness, inability to detect contrast, and other symptoms that reduce vision. eSight is able to significantly corrects these issues by using a high-speed camera, video processing software, a computer processor and the high quality video OLED screens to project a real-time image on the inside of the glasses, allowing people to see.
eSight requires considerably less training than the Argus II. It is intuitive, but as with learning anything new, the more you use it the easier it is to use. It is best to practice on a daily basis.
CentraSight from VisionCare Ophthalmic Technologies
The CentraSight uses a tiny telescope that is implanted inside the eye. The telescope implant was created to improve for people with end-stage age-related macular degeneration (AMD). The tiny telescope – about the size of a pea – is implanted inside one eye, behind the iris and is barely noticeable in your eye.

In end-stage AMD, the macula, where central vision occurs, is degenerated in both eyes without any healthy macular areas left for detailed central vision. There is no way for the individual to see around the central blind spot in their vision. It does not affect peripheral vision, which is blurry so you can’t use it to read, but you can use it to detect objects and movement.

Once implanted inside the eye, the tiny telescope works like a telephoto lens of a camera. It magnifies images onto the healthy areas of the retina to help improve central vision. Because the image is enlarged it reduces the effect the blind spot has on central vision. The surgical procedure is only performed on one eye because the peripheral (side) vision will be restricted in the eye with the telescope implant. This means the peripheral vision in the untreated eye will need to work in conjunction with the implanted eye. “A person uses the eye with the telescope implant for detailed central vision (such as reading “WALK” signs at a crosswalk). The other eye is used for peripheral vision (such as checking to see if cars are coming from the side).
Training with a CentraSight low vision specialist will be needed to develop the skills you need to use your new vision, such as how to switch your viewing back and forth between the eye with the telescope implant and the eye without the implant. You will still need to wear eye glasses and may need to use a hand-held magnifier with the telescope-implanted eye to read or see fine details clearly. However, in general, less magnification will be needed.
After eight years of research, a Canadian optometrist, Dr. Gareth Webb, has invented a tiny bionic lens that is able to enhance eyesight so that an individual can see three times better than the sharpness of 20/20 vision. The Ocumetics Bionic Lens is a button-shaped lens that can be injected into the eye in eight minutes in a procedure identical to cataract surgery.
As people get older, the lens inside the human eye becomes cloudy over time, causing blurred vision, known as cataracts. The Bionic Lens would be inserted, replacing the person’s clouded lens, similar to the intraocular lenses currently used in cataract surgery.
The Bionic Lens features a patented Ocumetics camera optics system, which is a tiny bio-mechanical camera that is able to shift focus from a close range object to optical infinity – as far as the eye can see – much faster than the human brain.
This device is still not available to the public, but Webb is hopeful that clinical trials will start soon. Depending on regulatory processes in each country, Webb hopes the Bionic Lens will be commercially available by 2017.
11/10/15
 Susan DeRemer, CFRE
Susan DeRemer, CFRE
Vice President of Devlopment
Discovery Eye Foundation
The Importance of An Eye Exam
Why You Need An Eye Exam
The end of the year is fast approaching – when was the last time you had an eye exam? Was it a comprehensive eye exam?
To keep your eyes healthy and maintain your vision, the American Optometric Association (AOA) recommends a comprehensive eye exam every two years for adults ages 18 to 60, and annual exams for people age 61 and older. However, if you have a family history of eye disease (glaucoma, macular degeneration, etc.), diabetes or high blood pressure, or have had an eye injury or surgery, you should have a comprehensive exam every year, unless otherwise indicated by your doctor.
Also, adults who wear contact lenses should have annual eye exams.
An important part of the comprehensive eye exam is the dilated eye exam to look inside your eye. Drops are placed in each eye to widen the pupil and allow more light to enter the eye. This gives your doctor a clear view of important tissues at the back of the eye, including the retina, the macula, and the optic nerve. This allows for early diagnosis of sight-threatening eye diseases like age-related macular degeneration, diabetic retinopathy, glaucoma, etc.
To better understand the importance of the dilated eye exam, here is a video from the National Eye Institute (NE) that explains what to expect.
At the end of your comprehensive eye exam your doctor should raise any concerns he has with you. But it is up to you to be prepared to react and ask questions for peace of mind and to help save your vision.
Questions To Ask After Your Eye Exam
It is always important to know if anything about your eyes have changed since your last visit. If the doctor says no, then the only thing you need to know is when they want to see you again.
If the doctor says the have been some minor changes, you need to know what questions to ask, such as:
- Is my condition stable, or can I lose more sight?
- What new symptoms should I watch out for?
- Is there anything I can do to improve or help my vision?
- When is the next time you want to see me?
If the doctor sees a marked change in your vision or give you a diagnosis of eye disease, you would want to ask:
- Are there treatments for my eye disease?
- When should I start treatment and how long will it last?
- What are the benefits of this treatment and how successful is it?
- What are the risks and possible side effects associated with this treatment?
- Are there any foods, medications, or activities I should avoid while I am undergoing this treatment?
- If I need to take medication, what should I do if I miss a dose or have a reaction?
- Are there any other treatments available?
- Will I need more tests necessary later?
- How often should I schedule follow-up visits? Should I be monitored on a regular basis?
- Am I still safe to drive?
Your vision is a terrible thing to lose, but with proper diet, exercise and no smoking, along with regularly scheduled eye exams, you improve your chances of maintaining your sight.
11/5/15
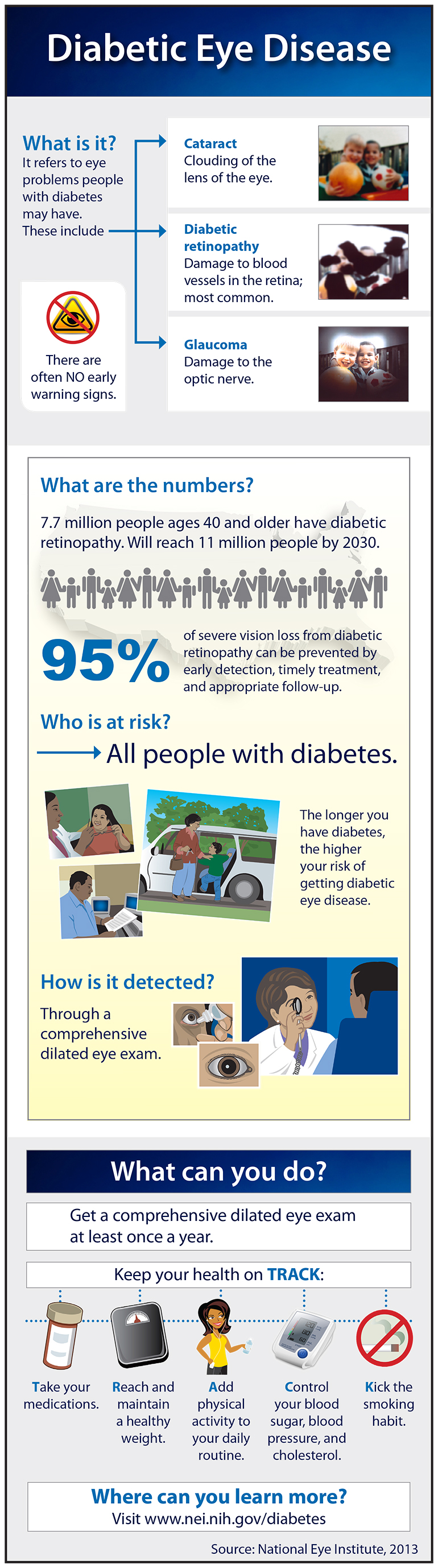
Diabetic Eye Diseases
November is National Diabetes Month. Diabetes is a controllable condition that is growing in the US. In adults 20 and older more than one in 10 people have diabetes, while in seniors (65 and older) that number increases to more than one in four.
Diabetic Eye Diseases
One of the eye diseases that can result from diabetes is diabetic retinopathy, which will affect approximately 11 million people by 2030. Check the infographic below to learn more about diabetic eye diseases.
11/3/15
 Courtesy of the National Eye Institute (NEI), a part of NIH.
Courtesy of the National Eye Institute (NEI), a part of NIH.