Just like any other organ in the body, the retina needs a healthy blood supply to function properly. When a blood vessel in the retina becomes blocked, sudden loss of vision can occur. Such blockages, known as retinal vascular occlusions, often occur in older adults. Because there are effective treatments available, seeing a specialist promptly can prevent further problems or even restore vision.
Retinal arterial occlusions
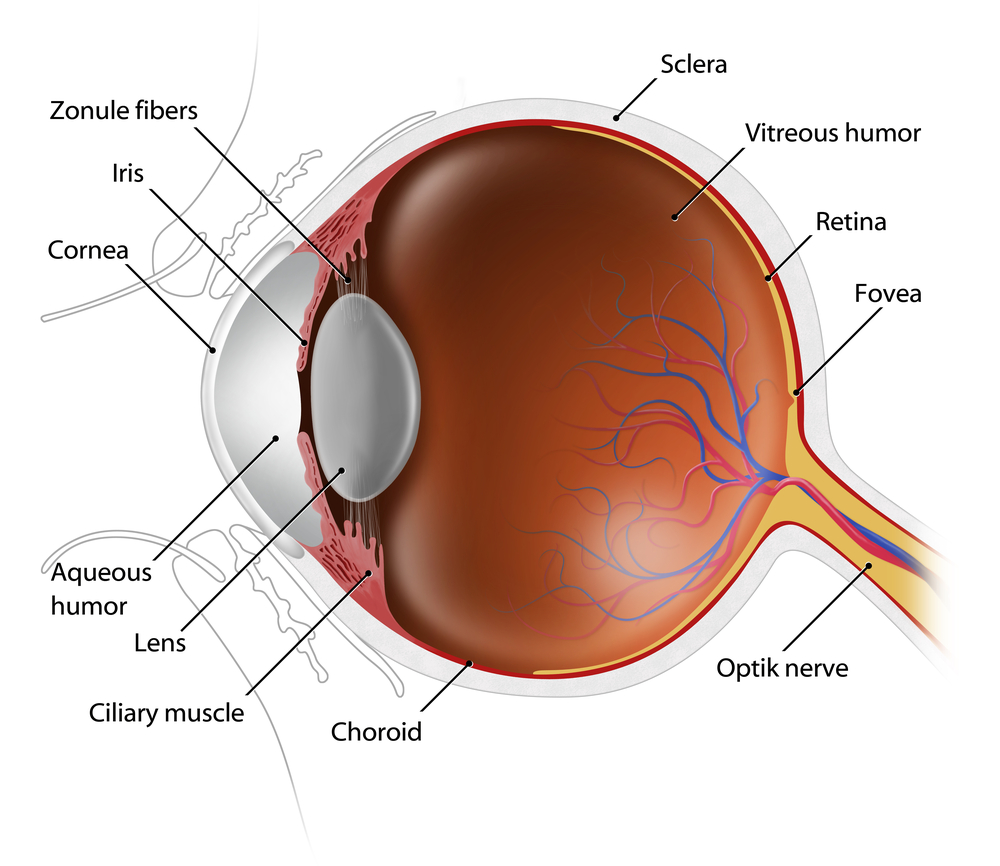
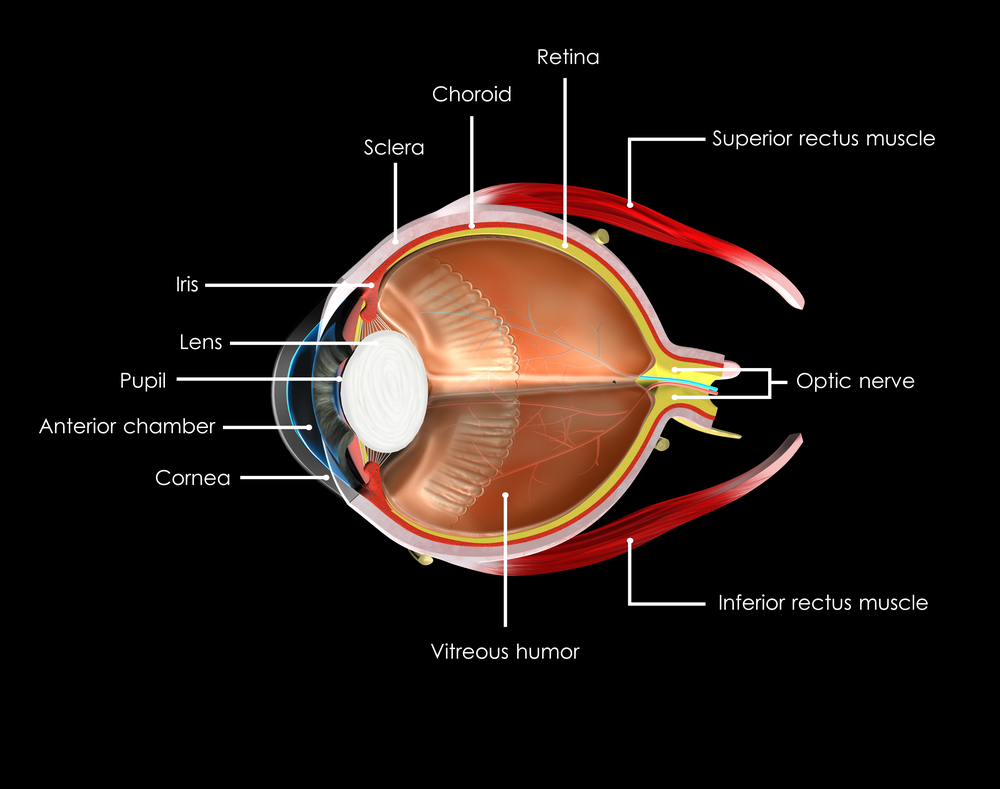
Arteries are the vessels that bring fresh blood containing oxygen and nutrients to different parts of the body. The artery that supplies the retina is known as the central retinal artery. After it enters the eye, the central retinal artery splits up into branch retinal arteries that serve different areas of the retina.
Symptoms
The symptoms of a central retinal artery occlusion include a sudden, painless loss of vision in one eye. Because the circulation to the entire retina is disrupted, the vision loss is profound and encompasses the entire field of vision. In contrast, a branch retinal artery occlusion only leads to loss of vision in a part of the field of vision. This is because only part of the retinal circulation in compromised. Similar to a central retinal artery occlusion, a branch retinal artery occlusion is also typically sudden and painless.
Evaluation
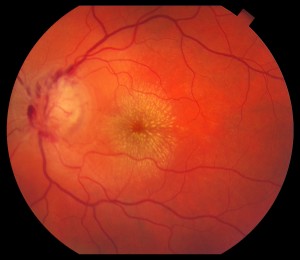
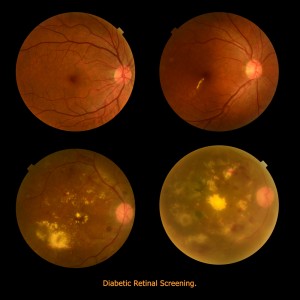
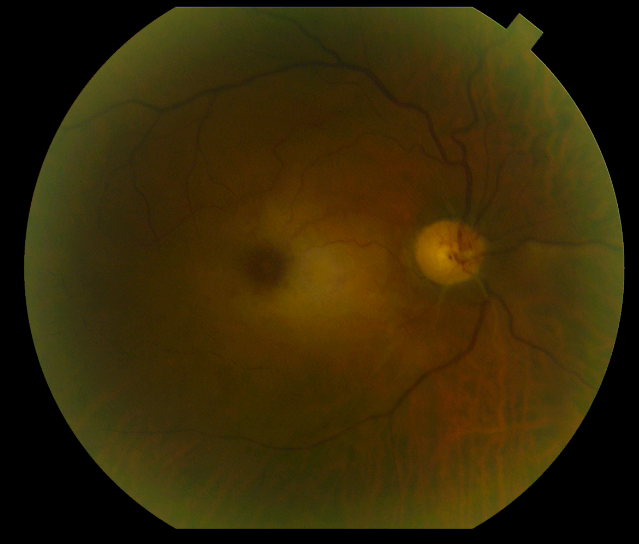
Retinal arterial occlusions can usually be diagnosed simply by examining the retina. Often, the retina is whitened in the area of the occlusion due to the lack of blood flow. Most arterial occlusions occur in patients with diseases such as high blood pressure or diabetes. On occasion, fragments of cholesterol or blood clots can be cause of the occlusion. Therefore, the treating physician will usually order tests looking for the source of these deposits in the carotid arteries or the heart. Another important cause of central retinal artery occlusions is a condition known as temporal arteritis. Temporal arteritis is an inflammatory disorder that can also produce fever, pain, or weight loss. Blood tests are ordered if temporal arteritis is suspected.
Unfortunately, there is no proven, reliable treatment for retinal arterial occlusions at this time. Various methods including hyperbaric oxygen, ocular massage, and anterior chamber paracentesis may or may not be effective if the occlusion is treated right away. However, if the occlusion is due to temporal arteritis, treatment with corticosteroids is effective at preventing loss of vision in the other eye. An unwanted, late complication of retinal arterial occlusions is neovascularization. Neovascularization refers to the growth of new, abnormal blood vessels in different parts of the eye that can result in bleeding, detachment of the retina, or glaucoma. Neovascularization is treated with laser or injections of anti-neovascular medications into the eye.
Retinal venous occlusions
After blood has passed into the eye through the retinal arteries, it leaves through the retinal veins. Blood travels first through the smaller, branch retinal veins and then enters the central retinal vein.
Symptoms
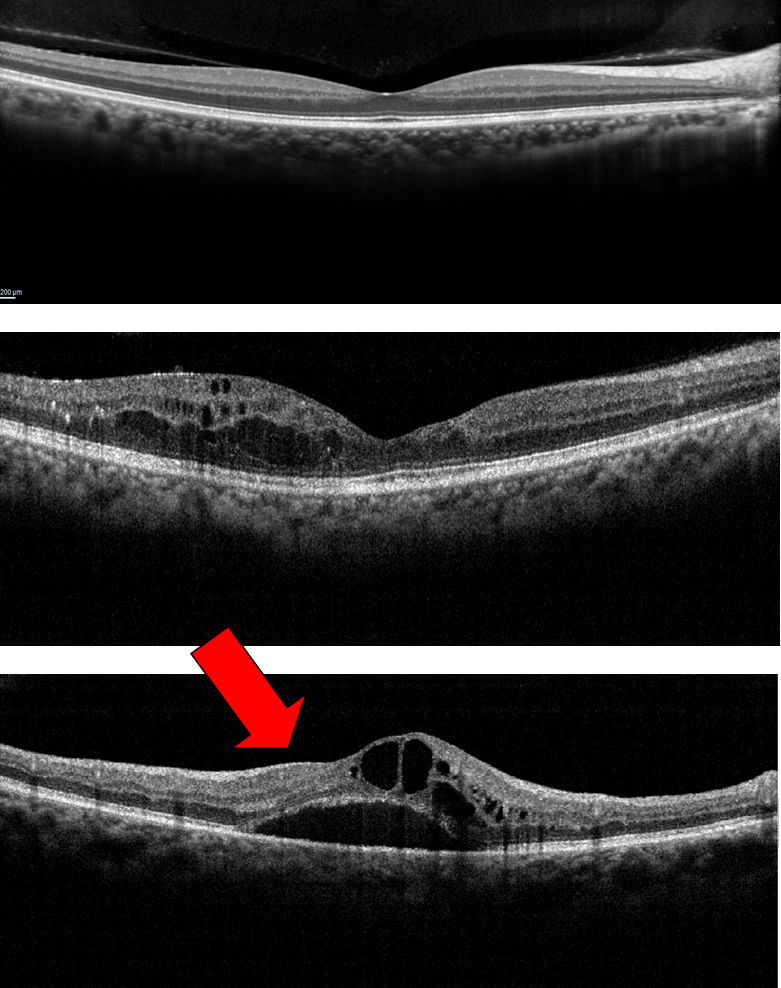
A central retinal vein occlusion usually causes sudden, painless vision loss in one eye. Unlike a central retinal artery occlusion, which causes profound vision loss, the visual deficit in a central retinal vein occlusion can range from mild to severe. More severe occlusions cause more severe deprivation of vital oxygen to retinal tissue. In addition, a central retinal occlusion can result in macular edema, swelling of the retina that also leads to blurred vision. A branch retinal vein occlusion usually leads to blurring of vision in only part of one eye. Like central retinal vein occlusions, branch retinal vein occlusions can vary in severity, but often result in macular edema as well.
Evaluation
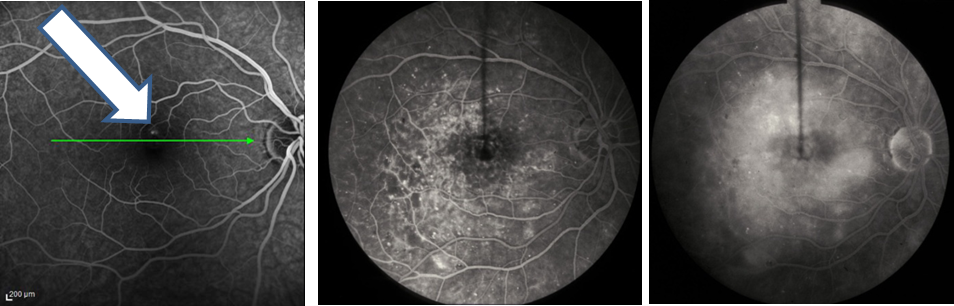
Retinal venous occlusions are also diagnosed by examining the retina. The blocked vein will appear dilated and engorged. In addition, the area of the retina served by that vein will contain hemorrhages or become swollen. To assess the amount of oxygen deprivation to the retina, a specialist will often recommend a fluorescein angiogram. The angiogram involves the injection of a yellow dye known as fluorescein intravenously. Subsequent photos allow visualization of the abnormal blood flow within the retina. In addition, optical coherence tomography is often performed to determine the amount of swelling within the retina.
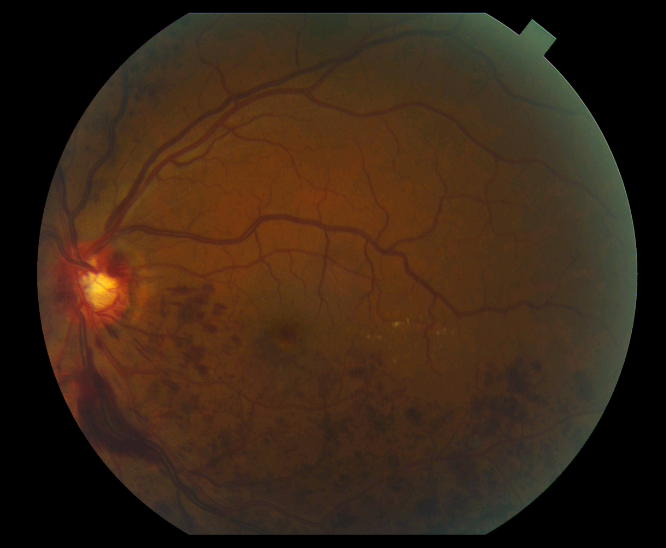
Treatment of retinal venous occlusions is largely aimed at decreasing swelling in the macula in hopes of improving vision. Currently, the most effective treatments involve injections of medication into the eye. FDA approved medications such as Lucentis and Eylea, that target abnormal levels of growth factors in the eye, can result in significant gains in vision in approximately two thirds of patients with branch retinal vein occlusions and half of patients with central vein occlusions. In addition, injectable steroid medications such as Ozurdex can also be effective, with approximately one third of patients having a significant visual gain. Laser can also be used to treat macular edema due to branch retinal vein occlusions. Keep in mind that these treatments likely need to be repeated on a routine basis or used in combination to achieve maximum benefits. If neovascularization occurs, it is treated as previously described in the section about retinal arterial occlusions.
In conclusion, occlusions of either retinal arteries or veins can cause significant visual impairment. Prompt evaluation and ongoing treatment with a retinal specialist can often improve and maintain vision.
9/24/15
 David Liao, MD, PhD
David Liao, MD, PhD
Retina-Vitreous Medical Group