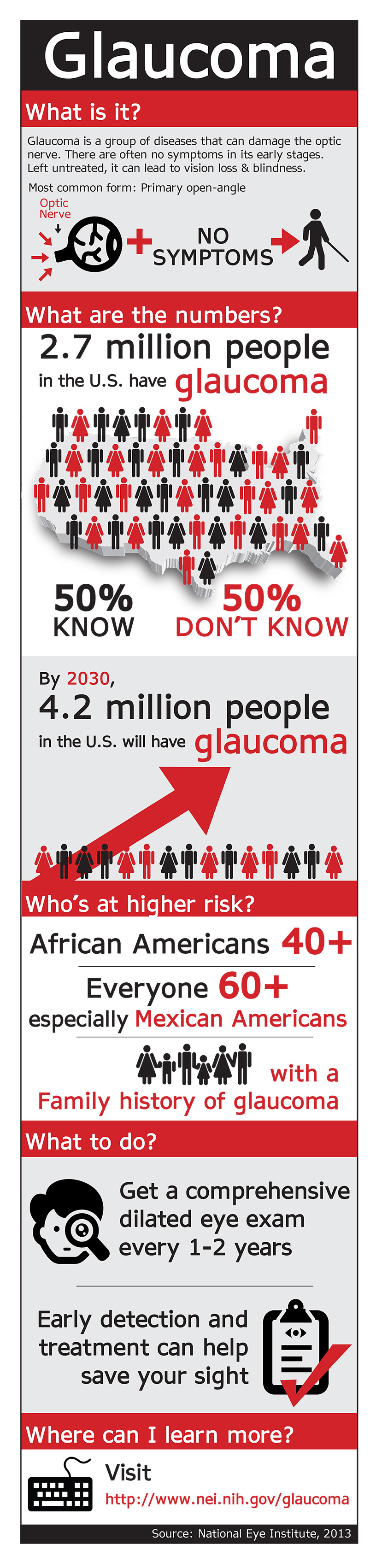
January is National Glaucoma Awareness Month. The National Eye Institute, through their education program NEHEP, have created this infographic to provide you with information you need to know about this blinding eye disease.
When adults reach their 40s, they often begin to notice small changes in their vision that can affect their daily lives and jobs. It could be difficulty in reading a book or working on a computer. This can be annoying, but it can often be addressed by seeing an eye care professional for comprehensive dilated eye exam. This allows the doctor to detect diseases and conditions that can cause vision loss and blindness and yet have no symptoms in their early stages.
Silent Thief of Sight – Glaucoma
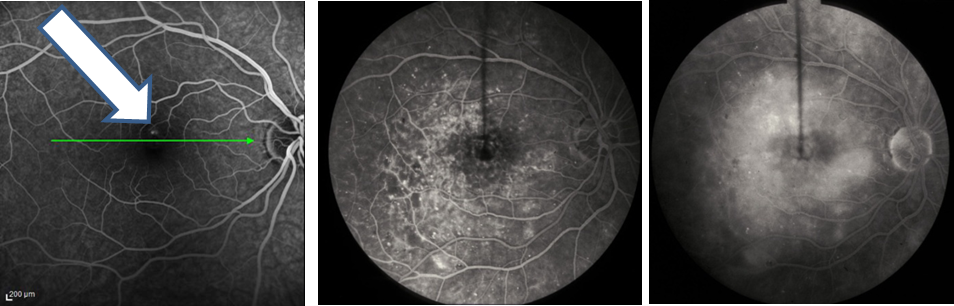
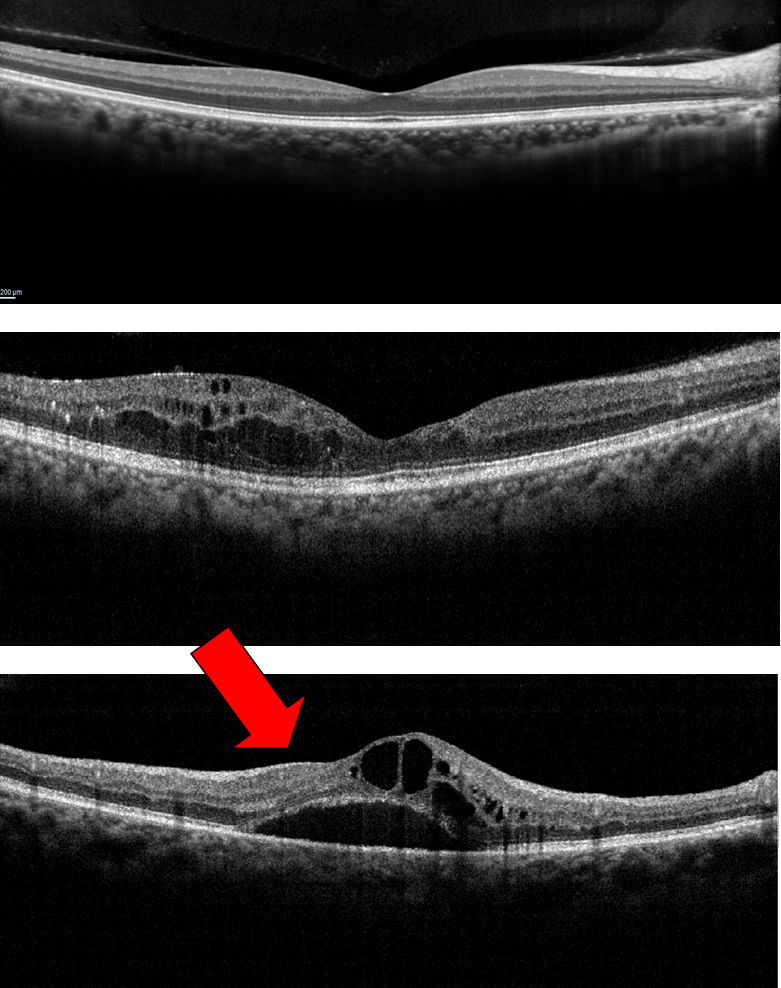
Glaucoma is one of these age-related eye diseases that has no early symptoms, which is why it is called the silent thief of sight. It is actually a group of diseases that can damage the eye’s optic nerve and result in vision loss and blindness. Open-angle glaucoma is the most common form disease.
In addition to an eye exam, you can reduce your chances of losing your vision to glaucoma by also:
- Live a healthy lifestyle that includes maintaining a proper weight, eating healthy foods, and not smoking.
- Know your family history to determine if you are at a higher risk for some eye diseases.
- Protect your eyes against harmful UV rays from the sun or your computer by wearing sunglasses when you are outdoors or computer glasses when using the computer for extended periods of time.
1/5/16
 Susan DeRemer, CFRE
Susan DeRemer, CFRE
Vice President of Development
Discovery Eye Foundation