Working long hours in front of the computer requires a fairly unchanging body, head and eye position which can cause discomfort. Correct working position, periodic stretch breaks, frequent eye blinking, artificial tears for lubrication are all very important. However, it’s not always easy to remember this when you are engrossed in work. Here are a few fun, free and easy-to-install “break reminders” to help: 
Workrave is break reminder program that alerts you to take “micro-pauses” and stretch breaks.
Take Your Break is another break reminder designed to prevent or minimize repetitive strain injury, computer eye strain and other computer related health problems. It has a friendly interface and a tray icon status indicator. It runs quietly in the background, monitoring your activity and reminding you to take regular breaks.
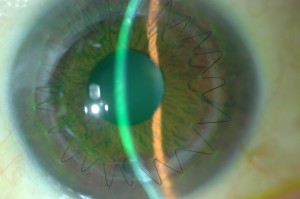
And remember to blink. Blinking cleans the ocular surface of debris and flushes fresh tears over the ocular surface. Each blink brings nutrients to the eye surface structures keeping them healthy. The flow of tears is responsible for wetting the lower third of the cornea. This is very important in KC, since this area is generally below the bulge of the cone and in many cases irritated by wobbly RGP lenses. Maybe your job requires hours of work at a computer. Maybe you like to spend your free time surfing the internet. Whatever the reason, your body is probably feeling the effects of spending too much time staring at a computer monitor, which could result in Computer Vision Syndrome (CVS). The most common symptoms are: eye strain, dry or irritated eyes,redness in eyes,difficulty in refocusing eye,neck pain,double vision,blurred vision, fatigue, and headaches.
Please join us on Thursday when Dr. Bezalel Schendowich will be providing a detailed insight into the importance of blinking, going beyond computer usage.
 Cathy Warren, RN
Cathy Warren, RN
Executive Director
National Keratoconus Foundation