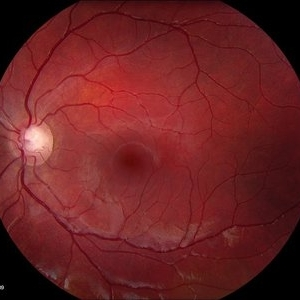
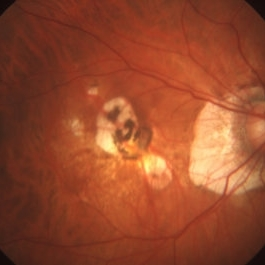
While there is still no concrete answer as to why some do not develop age-related macular degeneration (AMD) and other’s do, significant studies have proven the importance of a healthy diet and the mitochondria.
AMD is the leading cause of vision loss for those over 60 years of age in the developing countries. For decades we have studies that show the genetics and environmental factors associated with AMD. There have been over 20 genetics modification associated with AMD but there is no single gene that “causes AMD in all cases.” The genes most highly associated with AMD are found in the complement system, an important system related to controlling the inflammation in our body. A change in the complement factor H (CFH) gene from a low risk gene to a high risk gene has been associated with 43% of those developing AMD.
However, some people who have this high risk CFH gene but never develop AMD. This leads us to believe that the genetics are not the entire answer. The other factor has to do with the environment. Smoking is the leading risk factor, along with aging, exposure to sunlight and higher body mass index (obesity). But again there are obese people that smoke and never develop AMD. So, while the environmental risk factors are important, they do not answer the entire question of “why do some people get AMD but others do not?”
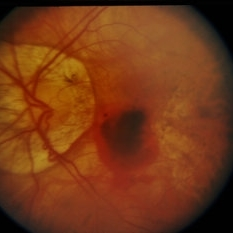
Recently, researchers have recognized that a major factor in the dry form of AMD is that the retinal cells begin to die off. Therefore, they have looked at important factors that keep cells alive. The mitochondria are one of the most important elements that protect the cells in the body. These subunits or organelles, produce energy for the cells, acting like batteries for the cells. And just like the batteries in a flashlight – if the batteries are not working then the flashlight dies. The same thing happens with cells – when the mitochondria are not healthy, then the cells eventually will die. Therefore to protect ourselves, it is important to keep the mitochondria healthy. One way to do this is to eat healthy foods. Over the past 20 years, the National Eye Institute (NEI) has conducted a series of studies that have identified foods and supplements that are good for the retinal cells and also the mitochondria.
 The National Eye Institute has recommended that people who are high-risk for developing AMD eat diets rich in green leafy vegetables, whole fruits, any type of nuts and omega 3 fatty acids. Many of these foods have anti-oxidant properties that help to “turn off” genes involved with inflammation, an important factor of retinal diseases. Salmon, mackerel and sardines have the highest levels of omega-3 fatty acids. An analysis that combined the data from 9 different studies showed that fish intake at least twice a week was associated with reduced risk of early and late AMD. Other studies show that Omega-3 fatty acids improve mitochondrial function, decreases production of reactive oxygen species (free radicals that damage cells) and leads to less fat accumulation in the body. The green leafy vegetables contain important protective macular pigments (carotenoids) called lutein and zeaxanthin that reduce the risk of AMD by 43%. High levels of lipid or fat deposits in the body (obesity) can “soak-up” the lutein and zeaxanthin so that they are not available to protect the retina.
The National Eye Institute has recommended that people who are high-risk for developing AMD eat diets rich in green leafy vegetables, whole fruits, any type of nuts and omega 3 fatty acids. Many of these foods have anti-oxidant properties that help to “turn off” genes involved with inflammation, an important factor of retinal diseases. Salmon, mackerel and sardines have the highest levels of omega-3 fatty acids. An analysis that combined the data from 9 different studies showed that fish intake at least twice a week was associated with reduced risk of early and late AMD. Other studies show that Omega-3 fatty acids improve mitochondrial function, decreases production of reactive oxygen species (free radicals that damage cells) and leads to less fat accumulation in the body. The green leafy vegetables contain important protective macular pigments (carotenoids) called lutein and zeaxanthin that reduce the risk of AMD by 43%. High levels of lipid or fat deposits in the body (obesity) can “soak-up” the lutein and zeaxanthin so that they are not available to protect the retina.
The goal is to increase the omega-3 fatty acid and carotenoid levels to protect the eye. Below is a list of foods that are eye healthy:
Foods that have lutein or zeaxanthin:
– 6mg/d of lutein and zeaxanthin – decreased
– Lutein/zeaxanthin content – ug/100g wet weight
– Kale, cooked – 15,798
– Spinach, raw – 11,935
– Spinach, cooked – 7,053
– Lettuce, raw – 2,635
– Broccoli, cooked – 2,226
– Green peas, cooked – 1350
Source: Johnson, et al 2005 Nutr Rev 63:9
To help kickstart an eye healthy diet, here is a list of “eye-healthy recipes” that provide nutritional support for the mitochondria and retinal cells.
Asparagus Soup
Kale Chips
Quinoa Collard Green Wraps with Summer Vegetables
Smoked Salmon Rillettes
Sources:
Geoffrey K. Broadhead, John R. Grigg, Andrew A. Chang, and Peter McCluskey Nutrition Reviews. Dietary modification and supplementation for the treatment of age-related macular degeneration VR Vol. 73(7):448–462
5/19/16