In the beginning…of contact lenses…there were scleral lenses…only.
In the year 1887 a great gift was given to the world of sufferers of distorted vision resulting from corneal tissue that was irregular in shape from disease or trauma.
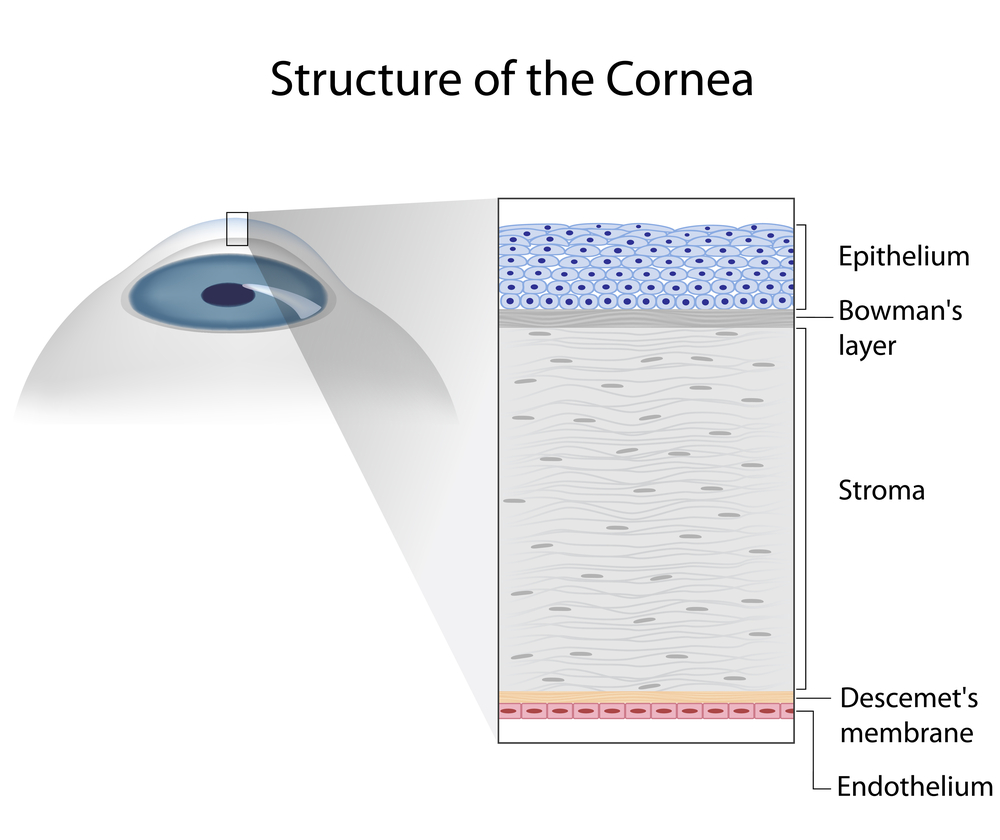
The contact lens was invented nearly simultaneously by physicians working separately in Germany and in France. Working from drawings of Leonardo da Vinci (1508) and ideas of the British astronomer Sir John Herschel (1828), August Müller and separately Adolph Fick and Eugene Kalt blew glass shells to fit the outer eye and to some extent remedy their visual difficulties. These lenses rested on the conjunctiva of the eye above the sclera or white of the eye and were thus the first scleral contact lenses — the first contact lenses of any sort.
What are Scleral Contact Lenses?
The design and manufacture of scleral lenses has been a story of technological development significant for improvement in comfort, material, and affinity for the ocular surface.
For many years the lenses were partially molded and partially ground from the material of which hard contact lenses are made: PMMA (poly-methyl methacrylate) known as Plexiglas or Perspex. To form these lenses, like tooth implants, a plaster cast is made from a negative mold prepared from dental impression putty. The plastic would be heated and given the shape of the fitting surface of the lens from the plaster cast and then the power and edge curves would be ground onto the outside surface of the lens. Later came preformed trial sets not unfamiliar to those which we use today.
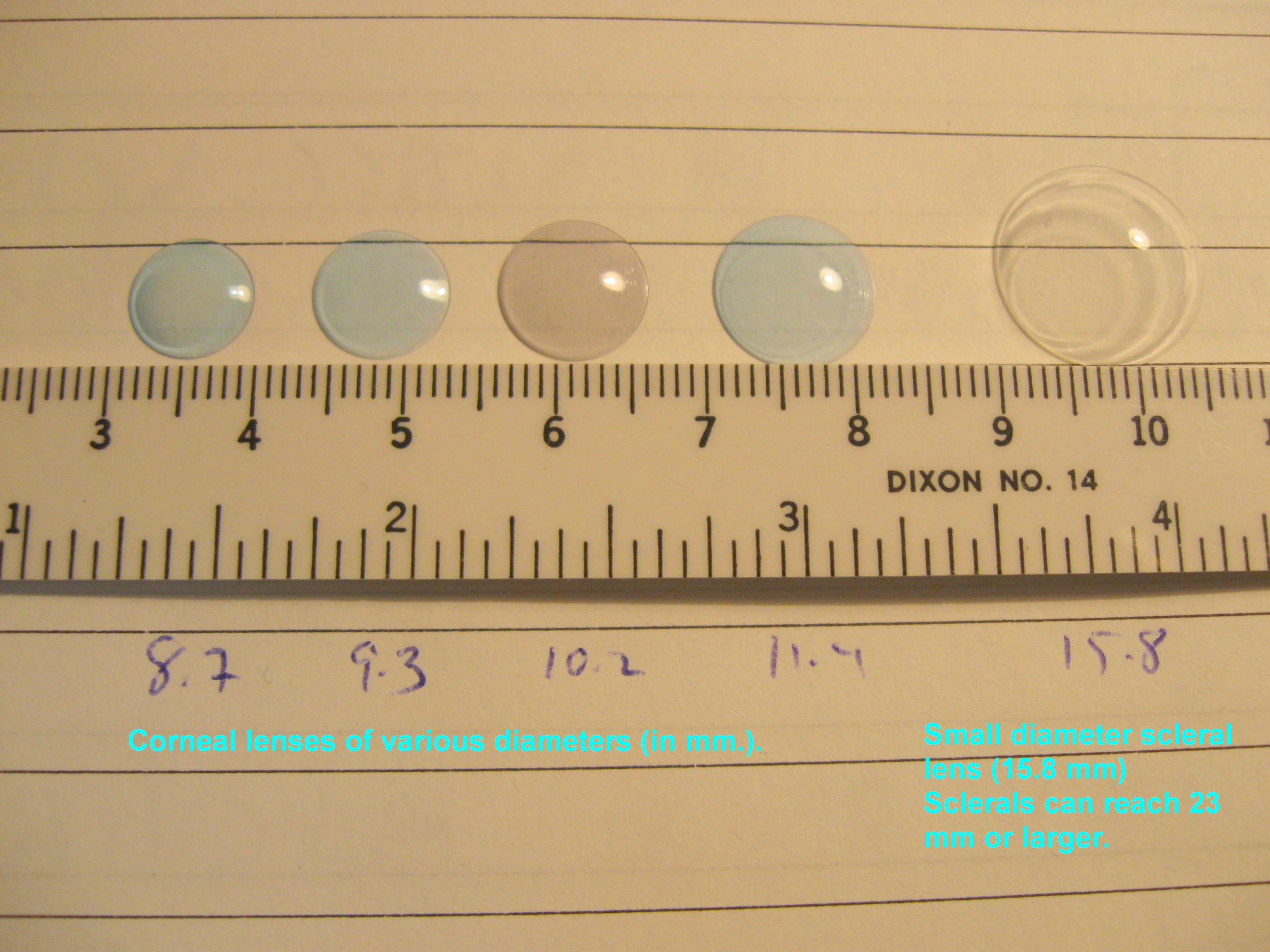
The current generation of scleral lens fitting began sometime in the last fifteen years with the mating of advanced corneal topography measurements, computer driven lathes and the observations of some very clever contact lens scientists. Proprietary designs of scleral lenses offering a variety of diameters, fitting philosophies, and multiple parameters are filling the gaps contact lens specialists have been wrestling with using smaller corneal contact lens designs for decades with less than optimal results. Most recently a firm has begun manufacturing lenses with a 3-D printer from an image generated from the eye. One eye…one lens, the lens is meant to fit like a fingerprint.
When discussing contact lens treatment, experts are experts because they agree that, any sort, size, or design of lens will have both positive and negative effects on the eyes and the tissues surrounding them. While it is true that many of the fitting and comfort issues confronted with corneal lenses of any size and design can be managed well with scleral designs, the scleral lens can also be difficult for some patients; for some eyes; for some conditions.
From the outset the larger size of the today’s scleral lens provides comfort on par with soft contact lenses for exactly the same reason: their size. Also, like soft contact lenses the scleral will not move around on the surface of the eye allowing the wearer a much more relaxed contact lens experience — there is no necessity to balance small corneal lenses between tense eyelids – vision can be enjoyed in any direction of gaze. The lenses will not fall off the eye and the increased size is a clear plus in finding a dropped contact lens.
On the other hand the quality of vision gained with scleral lenses specifically in cases of distorted corneae is far more comparable to that achievable with corneal GP lenses than with soft contact lenses in most cases.
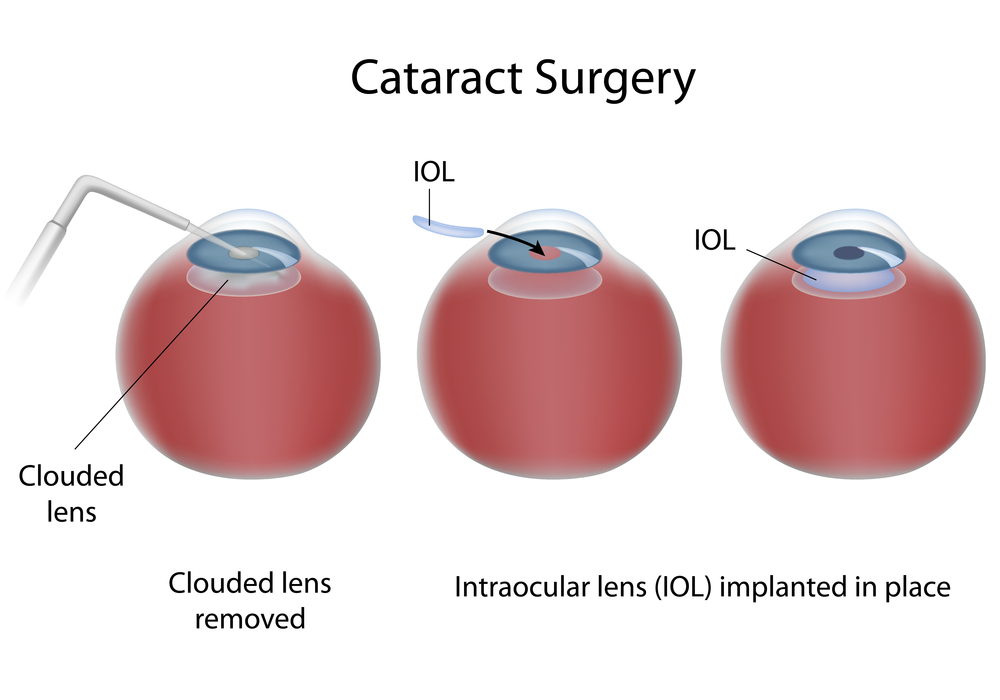
Over the years my keratoconus patients have benefited from a series of contact lens breakthroughs that have variously improved the quality of their vision, their comfort with contact lenses, or in some other way the health of their eyes. Some years ago I “re-invented” the piggy-back system of contact lens wear which I summarized in 2008 in an article published in the Contact Lens Spectrum. Piggy-backers would place their vision restoring firm contact lens on top of a disposable daily wear lens of minimal focusing power. The soft lens would reduce the sensation of the firm lens while in many cases preventing the contact lens from abrading the cornea. More recently I have been successfully moving patients to scleral lenses because there is certainly less bother (only one lens per eye) and far less worry over corneal abrasions as the lens rests on the conjunctiva over the sclera and maintains a fluid cushion over the cornea itself.
Scleral lenses are finding their place in the world of contact lens fitting primarily to remedy vision problems from very irregular or otherwise damaged corneae both those caused by developing disease and trauma through injury or surgery. More and more, these lenses are requested by patients with normal eyes who want to enjoy the benefits provided by these lenses while participating in sports or other activities.
Scleral lenses are renowned for their greater comfort. In many cases a correctly fitted lens can be worn for many waking hours. Many patients have found that they benefit from exchanging the fluid from the reservoir from time to time throughout the day. The fluid that fills the lens-cornea space is sterile, non-preserved normal saline or in some cases saline with a non-preserved tear substitute added when needed for improved comfort.
A proper care regimen for scleral lenses is not different from that for any other contact lens manufactured from a firm oxygen permeable material. The lenses require cleaning upon removal, soaking in a recommended solution appropriate to the material of the lens and a periodic treatment to remove protein deposits. Of course, the exact care specifications will vary from patient to patient according to the evaluation of their contact lens specialist.
Just like any lens modality, the fitting requires expertise. Many who fit and dispense contact lenses rely on boxed soft lenses for their patients. When corneae become distorted those lenses will hardly fill the need. Greater expertise is required to fit rigid corneal lenses needed for these more problematic surfaces. The decision of the corneal lens expert to move on to the world of larger lenses is not of the same magnitude as that from boxes to corneal GP lenses. The investment is more a matter of time spent in discussion with the manufacturer’s fitting consultants, some reading, a webinar or two and keeping up to date with the lens designs that are available.
I was not among the first to use the current generation of scleral lenses, but when the opportunity knocked some years ago, I realized the importance of this form of contact lens and I believe I have positively influenced the quality of life of many of my patients.
5/28/15
 Bezalel Schendowich, OD
Bezalel Schendowich, OD
Medical Advisory Board of the National Keratoconus Foundation
Fellow of the International Association of Contact Lens Educators
Clinical Supervisor & Specialty Contact Lens Fitter, Sha’are Zedek Medical Center, Jerusalem, Israel