Challenges Faced by Individuals Driving With Vision Loss
Overview
People of all ages often view driving as the key to independence. Individuals with vision loss are no exception. Three groups of people with vision loss who wish to acquire or maintain the privilege of driving include teenagers with a congenital or acquired visual impairment who have never driven, adults with the same who have never driven, and adults with an acquired visual impairment who have driven in the past but may lose their license because of their vision loss.  However, vision standards for driving vary from state to state, and this variation persists despite decades of research demonstrating that there is no absolute cutoff criteria in visual acuity or peripheral vision for safe versus unsafe driving. The fact that states have variable standards results in people with visual impairments not being able to be licensed in some states, including perhaps their own, while being able to be licensed in a neighboring state. Clearly, the ability of these individuals to safely operate a motor vehicle does not change when they cross a state line. Yet, to maintain at least some driving privileges, they may find themselves having to move to a different state.
However, vision standards for driving vary from state to state, and this variation persists despite decades of research demonstrating that there is no absolute cutoff criteria in visual acuity or peripheral vision for safe versus unsafe driving. The fact that states have variable standards results in people with visual impairments not being able to be licensed in some states, including perhaps their own, while being able to be licensed in a neighboring state. Clearly, the ability of these individuals to safely operate a motor vehicle does not change when they cross a state line. Yet, to maintain at least some driving privileges, they may find themselves having to move to a different state.
It is well known that many older drivers modify their driving norms to help keep themselves and others safe. For example, many older drivers voluntarily reduce or stop driving at night, in hazardous weather conditions, or on super highways. By limiting their driving, older drivers, particularly those with visual impairments, are able to continue operating their automobiles safely and efficiently in spite of reduced vision. This is important, considering the vast majority of older adults live in the suburbs or in rural areas where automobiles are required for transportation.
Maximizing Visual Capabilities
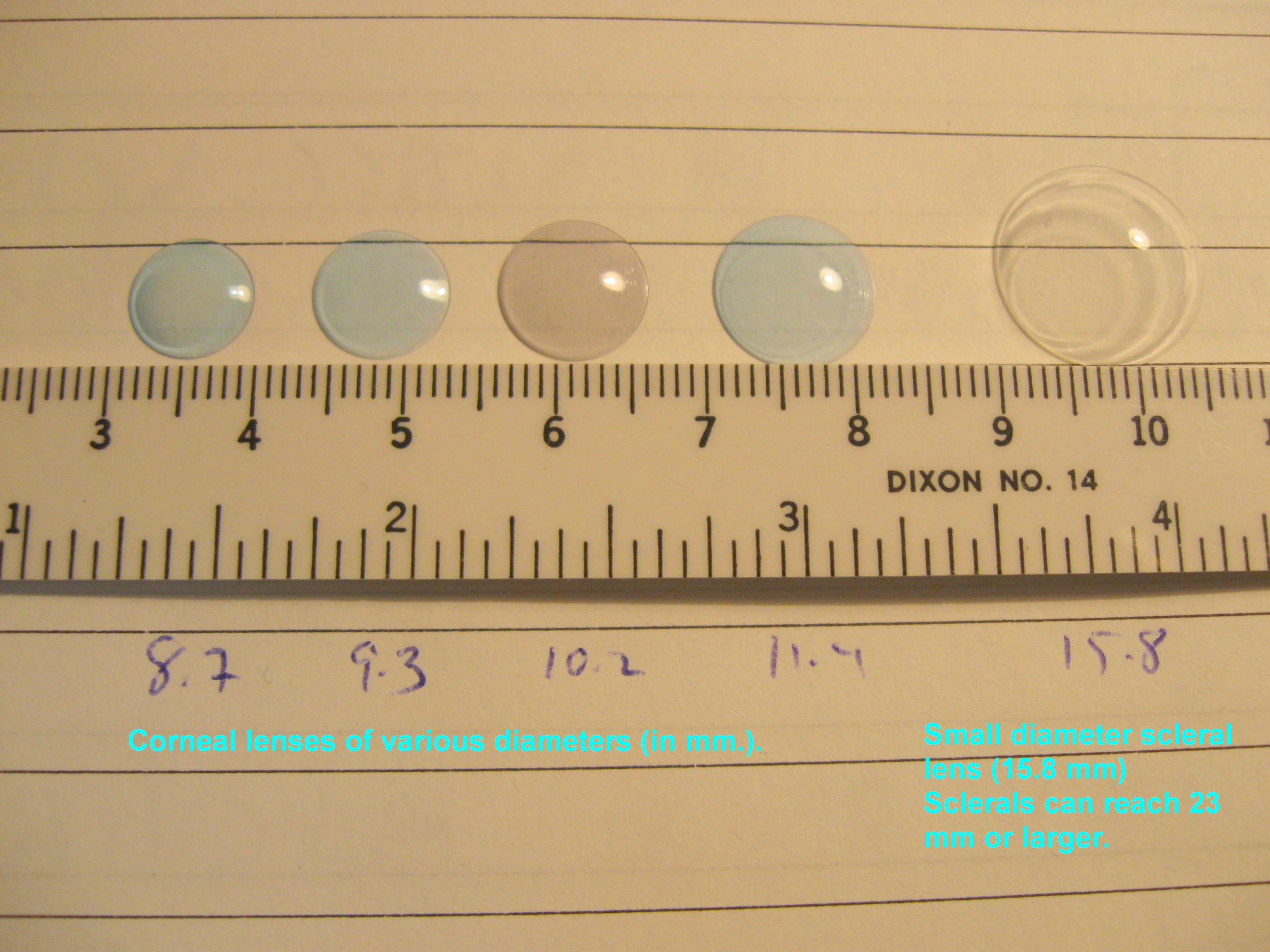
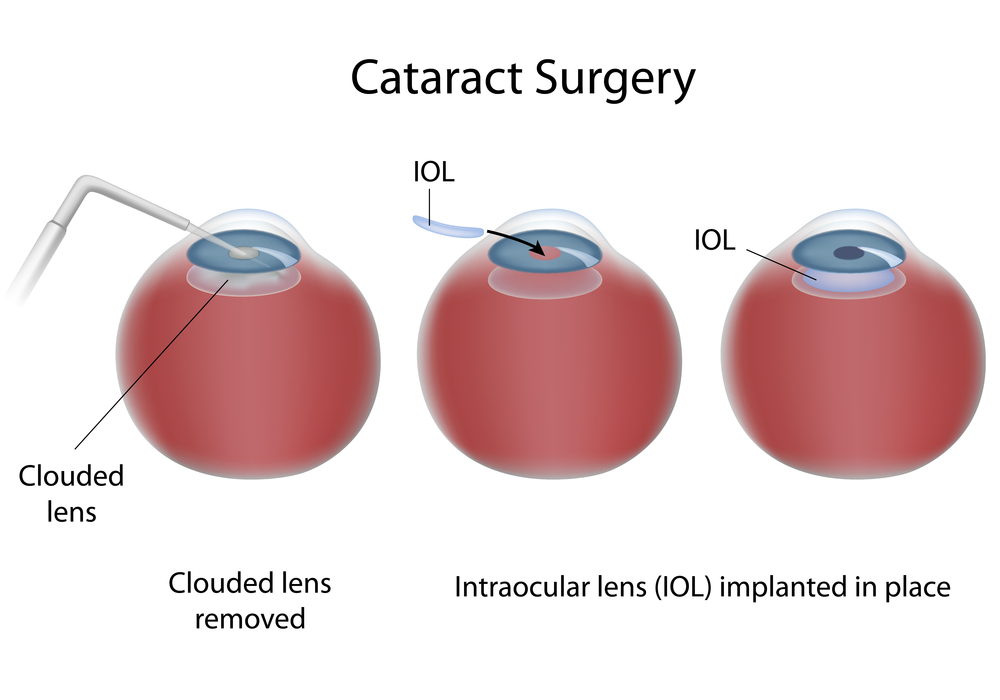
It is important for all individuals, but particularly for drivers who are visually impaired, to make sure their spectacle correction is up-to-date. Contrast enhancement and glare control with filtering lenses can also be of great benefit. Most drivers have experienced driving into the glare of the sun, while looking through a dirty windshield. Although wearing sunglasses and keeping windshields clean is not mandatory, they certainly help drivers see more easily and feel more comfortable when driving.
Maximizing Visual Attention
Human factors research has found that inattention blindness and the cost of switching contribute to or directly cause automobile mishaps. Inattention blindness refers to when a person’s attention to one activity undermines his or her attention to other activities. For example, when drivers focus on directional signs, their attention is not on what is happening on the road in front of them. The cost of switching refers to the time it takes a person to switch attention between different activities. A common example that causes driving mishaps is when drivers text while driving. When people focus on texting while driving, their response to the traffic around them is delayed.
Useful Field of View testing research has shown that the time it takes a person to process visual information, especially the complicated visual environment experienced each time a person drives, increases with age. With this in mind, decreasing or eliminating the time it takes older drivers or drivers with visual impairments to look for and visually process signage should help them maintain their concentration on the road ahead and the traffic around them.
A simple way to reduce or eliminate the need to look for directional signage is with the use of a Global Positioning System (GPS) device that uses spoken directions. Older drivers and drivers with visual impairments in particular should consider using a GPS device with spoken directions so that they are freed from the distraction of looking for/at road signs and can keep their attention on the traffic around them.
Finally, with the technology, such as adaptive cruise control and lane alert warnings, currently available in cars, it is expected that all drivers will be safer behind the wheel.
Final Considerations
A good driver is someone who has the ability to perceive change in a rapidly changing environment; the mental ability to judge and react to this information quickly and appropriately; and the motor ability to execute these decisions, along with the compensatory skills to compensate for some loss of ability in the other areas. Additionally, a driver’s familiarity with the driving environment and his or her past driving record should be taken into account when considering limiting driving activities or retiring from driving altogether.
For many drivers with vision loss, a limited driver’s license that allows them to drive during daylight hours, within a restricted radius of their home, and at lower rates of speed may be all they desire. However, there are times when an individual will need to retire from driving altogether because of vision loss or a combination of vision and cognitive changes. When this time comes, the individual needs to understand that retiring from driving is for his or her safety and the safety of others.
Finally, it is well known that vision loss in general, as well as the loss of driving privileges, can lead to feelings of hopelessness and depression. Fortunately, there are many things that can enhance the functional abilities of individuals with vision loss. To learn about available resources for individuals with vision loss, visit the National Eye Health Education Program low vision program page at www.nei.nih.gov/nehep/programs/lowvision.
7/9/15
 Mark Wilkinson, OD
Mark Wilkinson, OD
University of Iowa Carver College of Medicine
Chair of the National Eye Health Education Program Low Vision Subcommittee