It’s Healthy Vision Month! Make Your Vision Last a Lifetime.
When it comes to our health, we often visit our doctor or nurse regularly to make sure our bodies are healthy. But what about our eyes? They’re not always top of mind, but they’re just as important.
During Healthy Vision Month, held each May, the National Eye Institute (NEI) reminds you to make your eye health a priority and encourages you to take important steps to protect your sight.
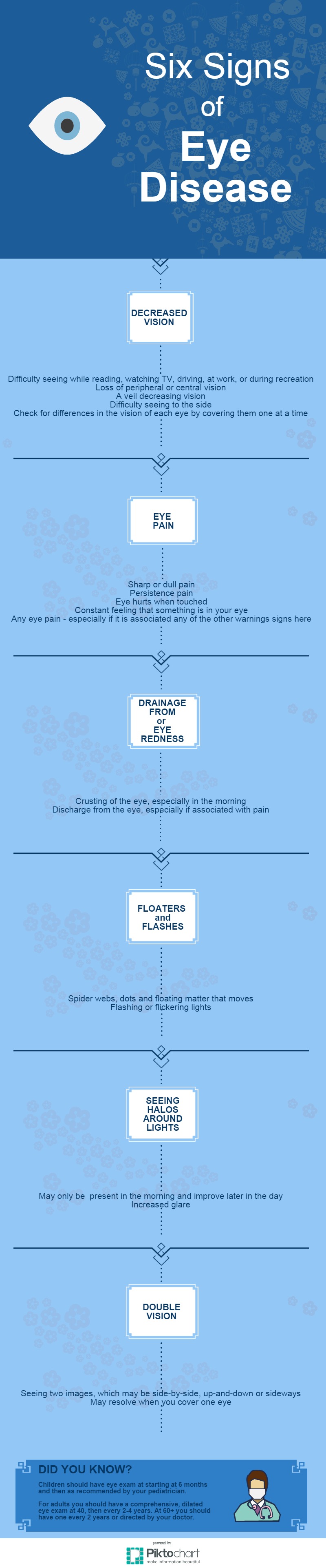
Get a dilated eye exam. Getting a dilated eye exam is the only way to detect eye diseases early, because with many, there are no warning signs. Talk to your eye care professional about how often you should have one. If you want to see what your eye care professional sees during a dilated eye exam, check out NEI’s new eye exam animation!

Live a healthy lifestyle. Eating healthy foods, maintaining a healthy weight, managing chronic conditions, and not smoking can lower your risk of eye disease.
Know your family history. Talk to your family members about their eye health history. It’s important to know if anyone has been diagnosed with an eye disease, since many are hereditary. This will help to determine if you are at higher risk for developing an eye disease yourself.

Use protective eyewear. Protect your eyes when doing chores around the house, playing sports, or on the job to prevent eye injuries from happening. This includes wearing safety glasses, goggles, safety shields, and eye guards that are made of polycarbonate.

Wear sunglasses. When purchasing sunglasses, look for ones that block out 99 to 100% of both UVA and UVB radiation, so you can keep your eyes healthy. Prolonged exposure to sunlight can increase your risk for getting an eye disease. A wide-brimmed hat offers great protection, too!
These steps can help you keep your eyes healthy and prevent vision loss and blindness from eye disease.
To learn more about Healthy Vision Month and find additional eye health information, visit www.nei.nih.gov/hvm.
5/5/15