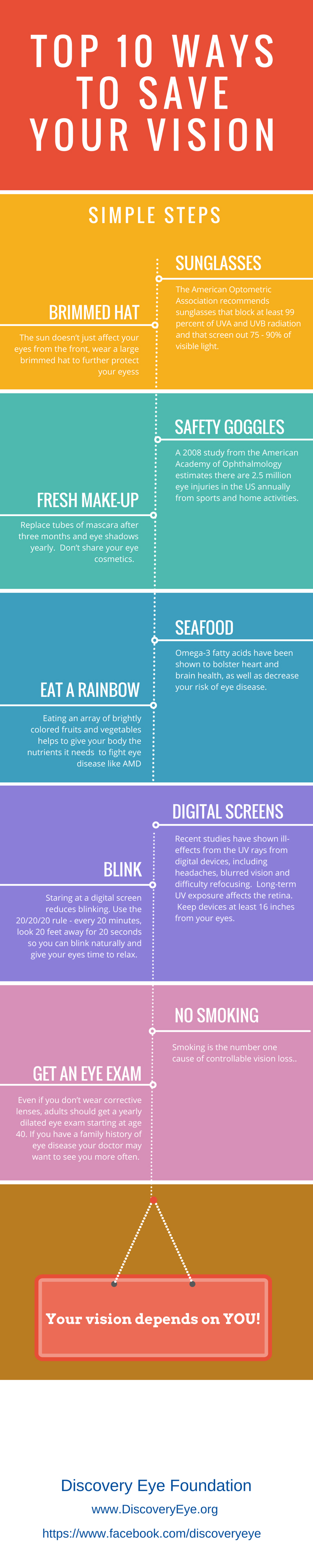
As we age, it’s normal to experience a change in eyesight, so it is important that we’re doing everything we can to keep our eyes clear and healthy. Eating a nourishing diet is not only good for your body, it’s also great for your eyes. There’s an easy way to improve your eye health: Start by making the same nutritious food choices that are good for your overall health and wellness.
The following vitamins, minerals and other nutrients are essential for good vision and may protect your eyes from sight-robbing conditions and diseases such as Age-Related Macular Degeneration (AMD).
Fruits and Vegetables
The nutrients in both fruits and vegetables provide antioxidants, which can help maintain healthier eyes. Fruits and vegetables also provide protection because many of their nutrients deliver antioxidants that our bodies cannot synthesize.
 For example, lutein and zeaxanthin are important antioxidants that help prevent degeneration in the lens and retina. Eating a diet rich in these carotenoids helps reduce the risk of AMD by fighting oxidation in the retinal cells of the eye.
For example, lutein and zeaxanthin are important antioxidants that help prevent degeneration in the lens and retina. Eating a diet rich in these carotenoids helps reduce the risk of AMD by fighting oxidation in the retinal cells of the eye.
Foods rich in lutein and zeaxanthin are typically dark-colored fruits and vegetables, including:
- spinach
- kale
- collard greens
- yellow corn
- carrots
- kiwi
- mangos
- melons
Omega-3 Fatty Acids
 Eating fatty fish, such as salmon, tuna, mackerel, and sardines, that are rich in omega-3 fatty acids also helps lower the risk of AMD. Omega-3 fatty acids are rich in docosahexaenoic acid (DHA), which is important for eye health and visual function. People with dry eye syndrome (i.e., low tear production) can benefit from a diet rich in omega-3 fatty acids because dry eye is linked to low levels of DHA.
Eating fatty fish, such as salmon, tuna, mackerel, and sardines, that are rich in omega-3 fatty acids also helps lower the risk of AMD. Omega-3 fatty acids are rich in docosahexaenoic acid (DHA), which is important for eye health and visual function. People with dry eye syndrome (i.e., low tear production) can benefit from a diet rich in omega-3 fatty acids because dry eye is linked to low levels of DHA.
However, studies have found that omega-3 fatty acid vitamin supplements may not provide as much protection. That means it’s better to eat the fish than just take omega-3 supplements. It’s important to note that heavy consumption of fish can contribute to high mercury levels (How Much is Too Much Mercury).
You can also find omega-3 fatty acids in plant-based sources, such as:
- nuts
- seeds (flax seeds and chia seeds)
- dark, leafy greens (romaine, arugula, spinach)
B Vitamins
Higher levels of B vitamins may lower your risk of developing AMD.
Foods that are high in vitamins B6 include:

- bananas
- chicken
- beans
- potatoes
- fish
- liver
- pork
Foods that are high in vitamin B12 include:

- dairy
- eggs
- meat
- poultry
- shellfish