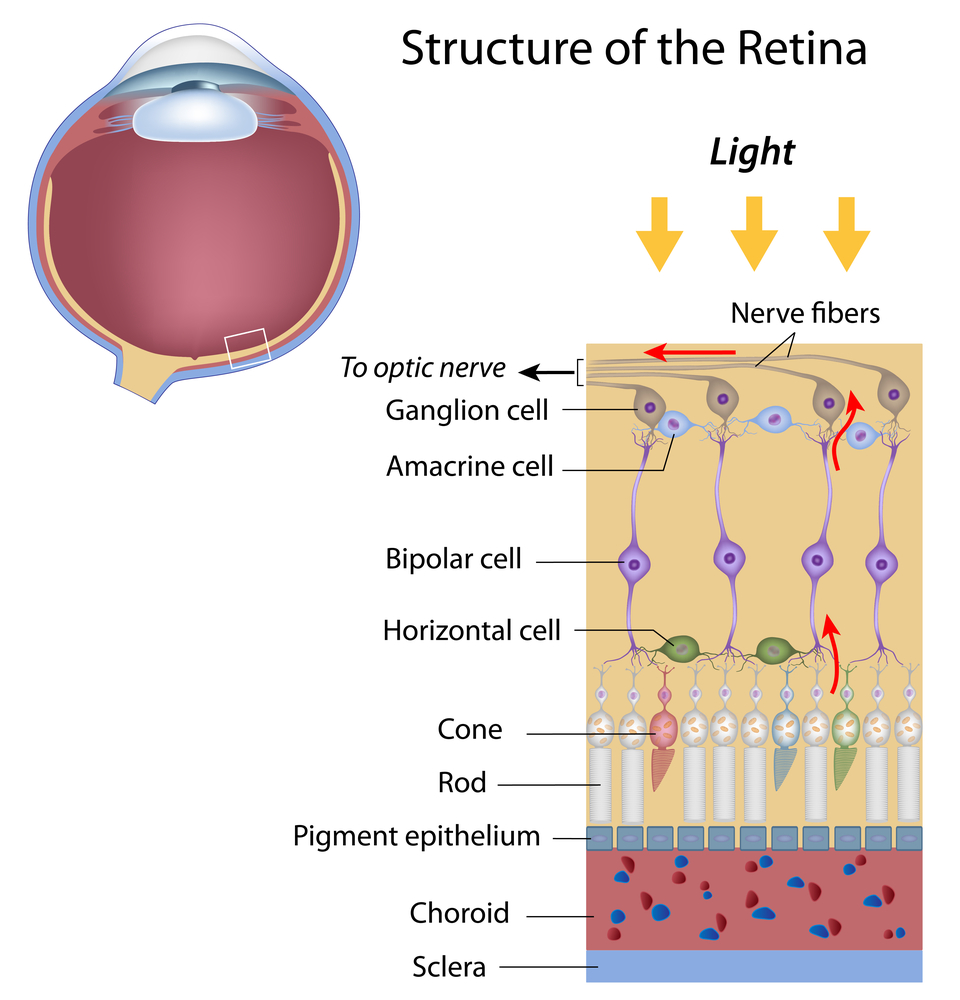
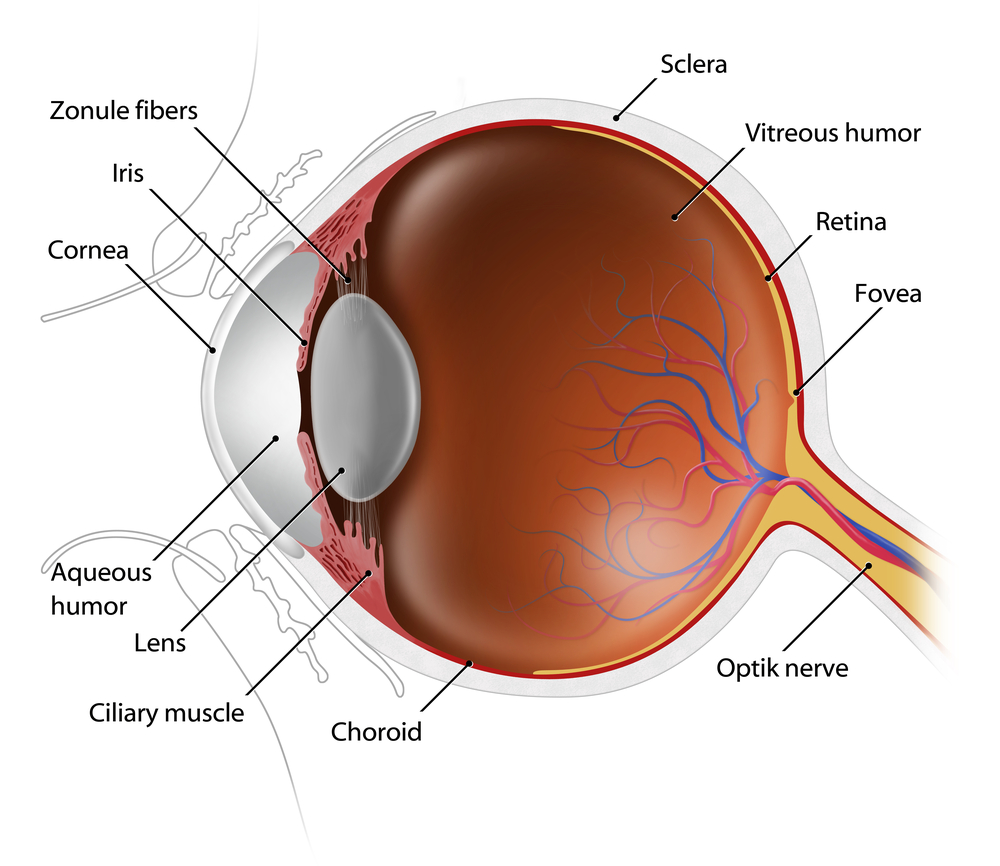
The retina at the back of the eye is essential for all vision. Each layer of cells in this tissue serves a specific purpose. As we prepare for Age-Related Macular Degeneration Awareness Month in February, a closer look at the layers of the retina and their function.
Layers of the Retina
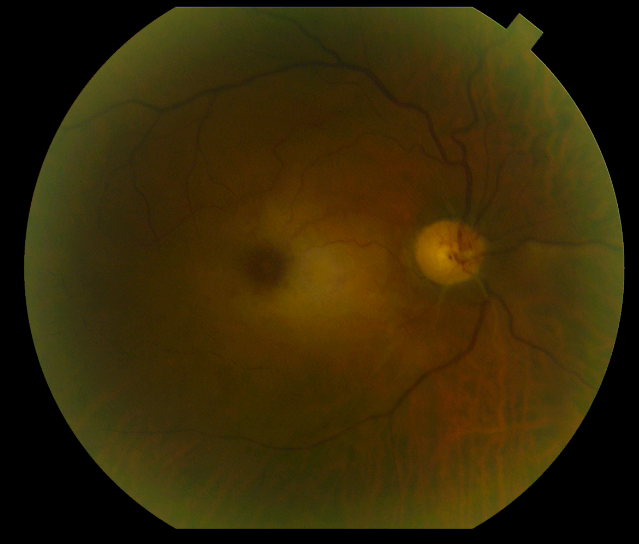
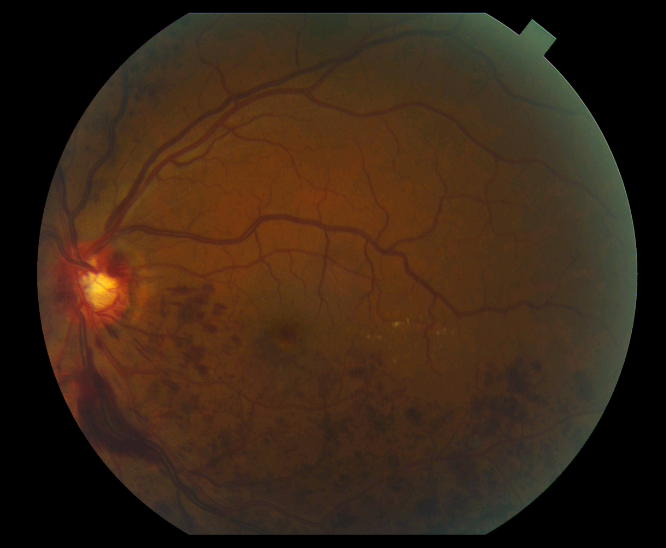
Choroid – This is made up of a layer of blood vessels that supply oxygen and nutrients to the retina. Defect in the CHM gene can cause choroideremia, leaky blood vessels can expand in the retina causing wet age-related macular degeneration (AMD) and diabetic retinopathy.
Retinal pigment epithelium – This is a single layer of cells that provide essential nutrition and waste removal for the photoreceptor cells. Accumulation of waste can lead to AMD and Stargardt disease.
Photorecptors – This is where the rods and cones are located that convert light into electrical signals. Rods help you with night and peripheral vision. Cones are more concentrated in the macula (the central part of the retina) and proved central and color vision. Death of the rods can cause vision loss called retinitis pigmentosa, while AMD is the loss of central vision.
Horizontal cells – These cells are connect to the photoreceptors that surround the bipolar connected photoreceptor cells and help the help integrate and regulate the input from multiple photoreceptor cells, increasing your visual acuity.
Bipolar cells – The dependence of each layer of the retina on each other is exemplified here. These cells take the electrical information from the photoreceptor cells and pass it along to other retinal cells.
Ganglion cells – These cells extend to form an optic nerve that conveys information to the brain and take the electrical information from the bipolar cells and process it to determine shapes, contrast and color. Glaucoma vision loss results from high intraocular pressure that affects the optic nerve, interrupting the signals to the brain.