Why Lutein & Zeaxanthin are vital for healthy vision.
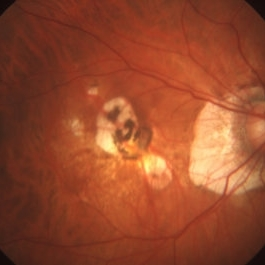
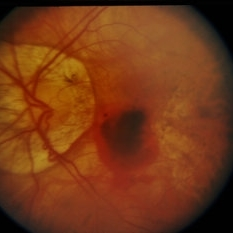
 Good nutrition is important to keep your eyes healthy. Researchers have linked two very important eye nutrients that play a key role in healthy vision. Lutein (LOO-teen) and Zeaxanthin (zee-ah-ZAN-thin), both are potent antioxidants and are best known for protecting your eyes and may reduce your risk for macular degeneration and cataracts.
Good nutrition is important to keep your eyes healthy. Researchers have linked two very important eye nutrients that play a key role in healthy vision. Lutein (LOO-teen) and Zeaxanthin (zee-ah-ZAN-thin), both are potent antioxidants and are best known for protecting your eyes and may reduce your risk for macular degeneration and cataracts.
Lutein and zeaxanthin are two types of carotenoids (kuh-RAH-teh-noids), which are yellow to red pigments found widely in vegetables and other plants and lutein is a yellow pigment, in high concentrations it appears orange-red.
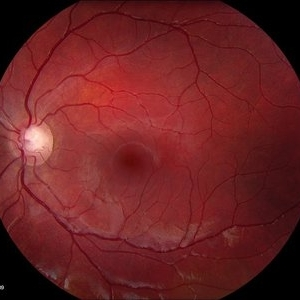
Both lutein and zeaxanthin can also be found in high concentrations in the macula of the human eye. The macula is essential for vision. Lutein and zeaxanthin work as important antioxidants in this area by protecting your eyes from harmful free radicals. It’s thought that a reduction of these antioxidants over time can impair eye health. Along with other natural antioxidants, including vitamin C, beta-carotene (vitamin A) and vitamin E, these important pigments guard the body from damaging effects of free radicals, which are reactive molecules that can destroy cells and play a role in many diseases. It is also believed that lutein and zeaxanthin in the macula block blue light from reaching the underlying structures in the retina, thereby reducing the risk of light-induced oxidative damage that could lead to macular degeneration (AMD).
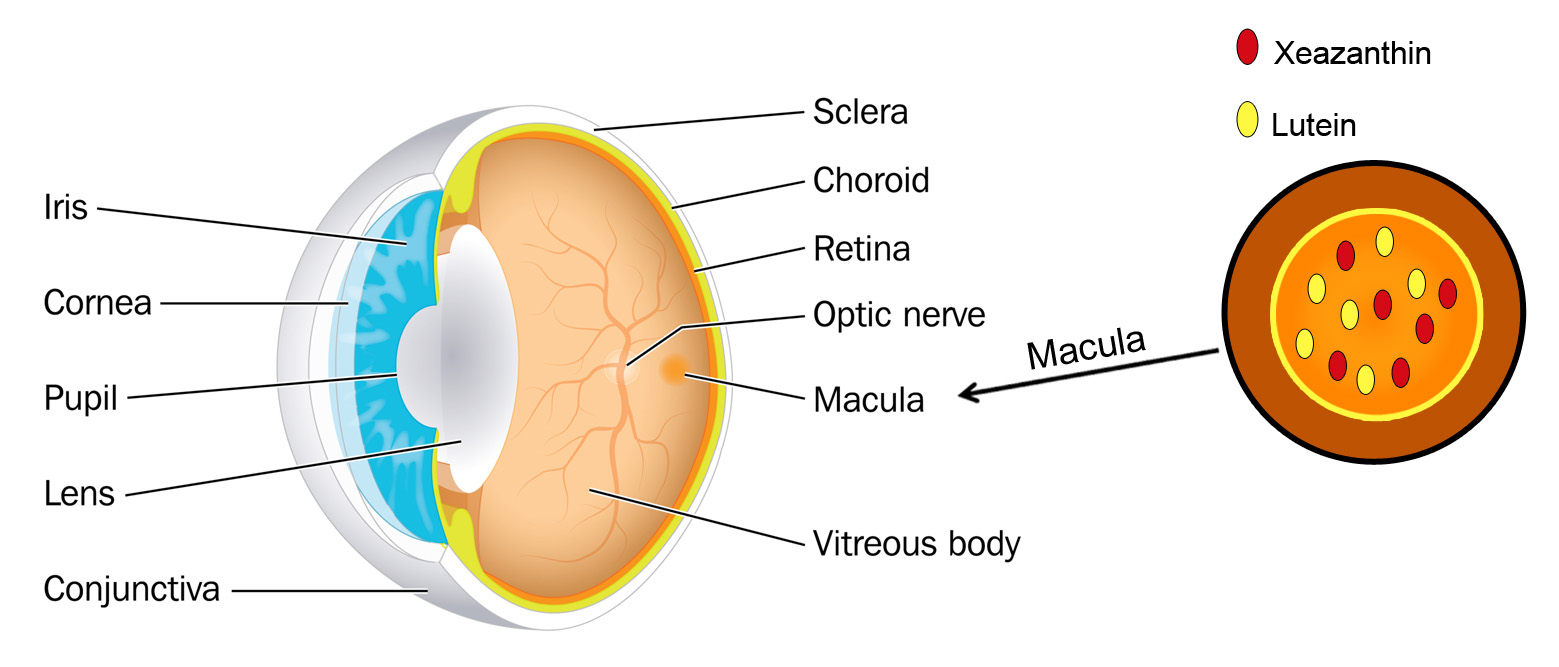
Unfortunately, the human body does not naturally make the lutein and zeaxanthin it needs. This is why getting daily amounts of lutein and zeaxanthin through your diet or nutritional supplements can help maintain good eye health.
Foods that Contain Lutein and Zeaxanthin
 Diets rich in these two nutrients may help hold off age-related eye diseases. The best natural food sources of lutein and zeaxanthin are green leafy vegetables and other green or yellow vegetables. Among these, cooked kale and cooked spinach top the list.
Diets rich in these two nutrients may help hold off age-related eye diseases. The best natural food sources of lutein and zeaxanthin are green leafy vegetables and other green or yellow vegetables. Among these, cooked kale and cooked spinach top the list.
Key sources of these carotenoids include kale, parsley, spinach, broccoli and peas. Orange juice, honeydew melon, kiwis, red peppers, squash and grapes are also good sources of lutein and zeaxanthin.
In addition, egg yolk may be an important source of lutein and zeaxanthin, as the high fat content of the yolk may improve the absorption of these nutrients.
For eye healthy recipes visit Eye Cook
Lutein and Zeaxanthin Supplements
Because of the benefits of lutein and zeaxanthin, many nutritional companies have added these carotenoids to their multiple vitamin formulas. Others have introduced special eye vitamins that are predominantly lutein and zeaxanthin supplements.
Some popular lutein and zeaxanthin supplements include:
- MacuHealth with LMZ3 (MacuHealth LLC)
- EyePromise Zeaxanthin (Zeavision)
- ICaps Eye Vitamin Lutein & Zeaxanthin Formula (Alcon)
- Macula Complete (Biosyntrx)
- MacularProtect Complete (ScienceBased Health)
- MaxiVision Ocular Formula (MedOp)
- OcuGuard Plus (TwinLab)
- Ocuvite (Bausch + Lomb
The source of lutein in many lutein supplements is marigold flowers, while for zeaxanthin it is often red peppers. If you choose a lutein and zeaxanthin supplement, make sure it’s a high quality product from a reputable dietary supplement company.
Be sure to keep in mind that individuals sometimes react differently to certain supplements, which can have unintended effects such as adverse reactions with medications. Consult with your physician or eye doctor before trying any vision supplements.

Remember that taking dietary supplements does not replace a healthy diet. Eating a well-balanced diet that includes plenty of fruits and vegetables usually is the best way to get the important eye nutrients you need.


 Tom Sullivan
Tom Sullivan The other day my daughter Blythe asked me which Christmas I consider to be my favorite. I had to think a minute, because as a family, the Sullivan’s have had some great ones. I was about to say the first time you and your brother Tom were old enough to really get into Santa, being absolutely sure that the fat man brought your presents right down the chimney. I was about to say that, and then I remembered.
The other day my daughter Blythe asked me which Christmas I consider to be my favorite. I had to think a minute, because as a family, the Sullivan’s have had some great ones. I was about to say the first time you and your brother Tom were old enough to really get into Santa, being absolutely sure that the fat man brought your presents right down the chimney. I was about to say that, and then I remembered.  Colorado, when our children were teenagers and our friend, the marvelous Betty White, joined us for a Christmas Eve sleigh ride none of us will ever forget. The night was perfect. It had snowed earlier that day, and the air had a feeling of Christmas that you could almost taste. Oh, sure, it was cold, but we were bundled up under tons of blankets as two beautiful Clydesdale horses with bells jingling took us through the woods to a magical barn where dinner would be served and carols sung.
Colorado, when our children were teenagers and our friend, the marvelous Betty White, joined us for a Christmas Eve sleigh ride none of us will ever forget. The night was perfect. It had snowed earlier that day, and the air had a feeling of Christmas that you could almost taste. Oh, sure, it was cold, but we were bundled up under tons of blankets as two beautiful Clydesdale horses with bells jingling took us through the woods to a magical barn where dinner would be served and carols sung.  Tom Sullivan
Tom Sullivan For 8 years I served as a member of the Academy of Ophthalmology’s Foundation Board. In that time we conducted a number of studies in all areas of vision preservation. The one that I believe was most meaningful occurred when we asked thousands of people to express what frightened them most in life. Frankly, I was really surprised at the results of the study. I was sure that people would say maybe stage four cancer, or ALS, or some other terminal disease would be the thing that would frighten them the most. I would have imagined that they might talk about the loss of a loved one or even the fear of a natural disaster. The results of the study were very clear. 62% of all the participants said that the loss of vision was the single most frightening possibility they would ever have to face.
For 8 years I served as a member of the Academy of Ophthalmology’s Foundation Board. In that time we conducted a number of studies in all areas of vision preservation. The one that I believe was most meaningful occurred when we asked thousands of people to express what frightened them most in life. Frankly, I was really surprised at the results of the study. I was sure that people would say maybe stage four cancer, or ALS, or some other terminal disease would be the thing that would frighten them the most. I would have imagined that they might talk about the loss of a loved one or even the fear of a natural disaster. The results of the study were very clear. 62% of all the participants said that the loss of vision was the single most frightening possibility they would ever have to face. Tom Sullivan
Tom Sullivan Costume Contact Lenses such as cat eyes or zombie may make your Halloween costume a bit more frightful although wearing those lenses without a prescription can be more terrifying, as it could result in vision loss or even blindness.
Costume Contact Lenses such as cat eyes or zombie may make your Halloween costume a bit more frightful although wearing those lenses without a prescription can be more terrifying, as it could result in vision loss or even blindness.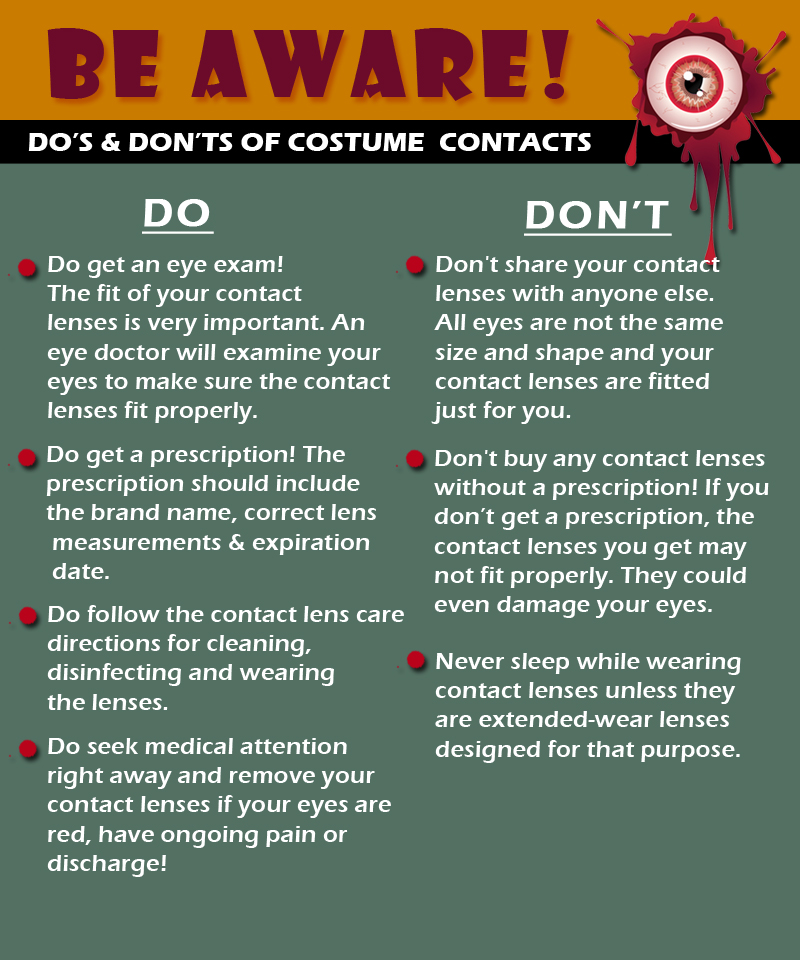

 Tom Sullivan
Tom Sullivan

 Be sure to start your holiday meal with a salad, it’s an excellent way to ensure that you and your guests get plenty of zeaxanthin and lutein, two nutrients that help protect your central vision. Adding kale, spinach, or romaine lettuce to salads helps your eyes absorb damaging blue light, combats the effects of cigarette smoke and pollution, and also decreases your risk of developing
Be sure to start your holiday meal with a salad, it’s an excellent way to ensure that you and your guests get plenty of zeaxanthin and lutein, two nutrients that help protect your central vision. Adding kale, spinach, or romaine lettuce to salads helps your eyes absorb damaging blue light, combats the effects of cigarette smoke and pollution, and also decreases your risk of developing  Turkey and lean beef, two of the main ingredients in many holiday meals, keep your eyes strong and healthy. Both foods are high in zinc, a nutrient important to the retina and the choroid layer under the retina.
Turkey and lean beef, two of the main ingredients in many holiday meals, keep your eyes strong and healthy. Both foods are high in zinc, a nutrient important to the retina and the choroid layer under the retina.  Zinc is essential for good night vision. Eating foods that are high in the nutrient can also reduce your risk of cataracts and AMD. Other foods that contain zinc include pork, dairy products, chick peas, black-eyed peas, crab, oysters, beans, spinach, mushrooms, cashews, and almonds.
Zinc is essential for good night vision. Eating foods that are high in the nutrient can also reduce your risk of cataracts and AMD. Other foods that contain zinc include pork, dairy products, chick peas, black-eyed peas, crab, oysters, beans, spinach, mushrooms, cashews, and almonds.  It wasn’t an old wives tale, it is true Carrots are good for your eyes! They contain beta carotene, a substance that turns into vitamin A when eaten. Eating carrots can benefit your night vision and could possibly reduce your risk of cataracts, AMD, and dry eyes. Other foods that contain beta carotene include pumpkin, sweet potatoes, and butternut squash. All great ingredients to include into your holiday feast.
It wasn’t an old wives tale, it is true Carrots are good for your eyes! They contain beta carotene, a substance that turns into vitamin A when eaten. Eating carrots can benefit your night vision and could possibly reduce your risk of cataracts, AMD, and dry eyes. Other foods that contain beta carotene include pumpkin, sweet potatoes, and butternut squash. All great ingredients to include into your holiday feast.  Fish contain omega-3 fatty acids, which can reduce your risk of developing AMD, dry eye, and glaucoma. Salmon, mackerel, flounder, tuna, halibut, herring, and sardines would be a great addition to your holiday meals.
Fish contain omega-3 fatty acids, which can reduce your risk of developing AMD, dry eye, and glaucoma. Salmon, mackerel, flounder, tuna, halibut, herring, and sardines would be a great addition to your holiday meals. Whole grains reduce your risk of heart disease, obesity, and type 2 diabetes and can also decrease your risk of AMD. Substituting whole grain flour for white flour in holiday breads and muffins is a simple way to boost your whole grain intake. Other good whole grain sources include wild rice, brown rice, popcorn, oatmeal, bulgur, barley, buckwheat, and couscous.
Whole grains reduce your risk of heart disease, obesity, and type 2 diabetes and can also decrease your risk of AMD. Substituting whole grain flour for white flour in holiday breads and muffins is a simple way to boost your whole grain intake. Other good whole grain sources include wild rice, brown rice, popcorn, oatmeal, bulgur, barley, buckwheat, and couscous.  Fruits high in vitamin C, such as strawberries and oranges, also offer important vision benefits. Vitamin C is an antioxidant, a substance that can prevent cell damage caused by free radicals. Vitamin C-rich foods help keep the collagen in your cornea healthy and reduce the risk of cataracts and AMD. You can also find vitamin C in grapefruit, kiwi, blueberries, peas, broccoli, and tomatoes.
Fruits high in vitamin C, such as strawberries and oranges, also offer important vision benefits. Vitamin C is an antioxidant, a substance that can prevent cell damage caused by free radicals. Vitamin C-rich foods help keep the collagen in your cornea healthy and reduce the risk of cataracts and AMD. You can also find vitamin C in grapefruit, kiwi, blueberries, peas, broccoli, and tomatoes.