10/9/14
What is the macula?
The eye is very much like a camera, taking light from the outside world and converting it into picture information that our brains perceive as vision. The retina is the light sensitive layer in the back of the eye that is very much like the film in that camera. The central retina, also known as the macula, is essential for crisp, high definition vision. Conditions that damage or distort the macula can therefore result in blurred or distorted vision. Two common conditions that affect the macula are macular puckers and macular holes.
What is a macular pucker or macular hole?
A macular pucker is a thin layer of scar tissue that forms on top of the retina. The amount of scar tissue can range from mild to severe. Mild macular puckers may be barely noticeable during an eye exam and resemble a fine layer of cellophane resting on the macula. More severe macular puckers can cause wrinkling or distortion of the macula. In contrast to a macular pucker, a macular hole is a small gap that extends through the entire thickness of the macula.
What are the symptoms of a macular pucker or a macular hole?
At first, a macular pucker may lead to mild blurring of the central vision. Because the problem involves the back of the eye, glasses will not completely restore vision. More severe macular puckers may result in wavy or distorted vision. For instance, objects that normally appear straight, such as venetian blinds or a printed line of text, might appear to have a dip or bend in the center. Small macular holes can cause similar symptoms of blurring or distortion. Larger macular holes often result in a central blind spot. This can also result in straight lines appearing broken or having a piece missing in the middle. Patients with a macular pucker or hole do not normally experience difficulty with peripheral vision.
What can cause a macular pucker or macular hole?
Recall that a macular pucker is a scar tissue. Anything that causes scar tissue, such as trauma or inflammation in the eye, can result in scar tissue and hence a macular pucker. Certain diseases that affect the retinal blood vessels such as diabetes can also cause a macular pucker to form. However, one of the most common causes of macular pucker is simple aging of structures within the eye. As the eye ages, the clear jelly that fills it, called the vitreous gel, shrinks. When enough shrinkage occurs, the vitreous gel detaches from its normal position adjacent to the retina. This process of vitreous detachment can cause microscopic damage or inflammation leading to macular pucker formation. In some cases, the vitreous gel does not detach cleanly from the retina. Instead it can put traction on the macula, pulling its delicate structures apart in the center, resulting in a macular hole.
How are macular puckers and macular holes diagnosed?
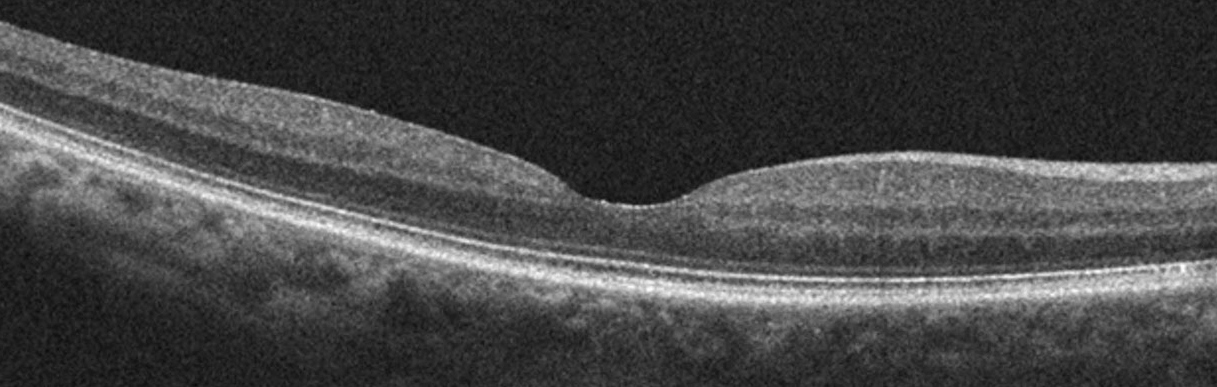
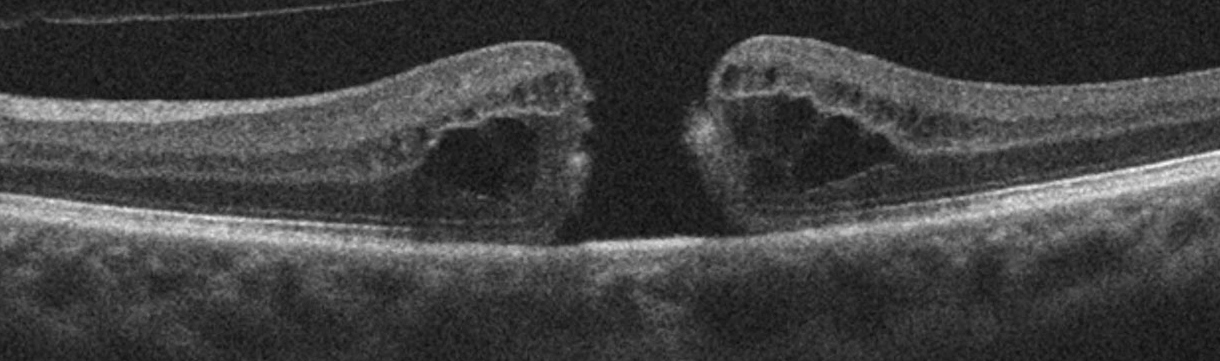
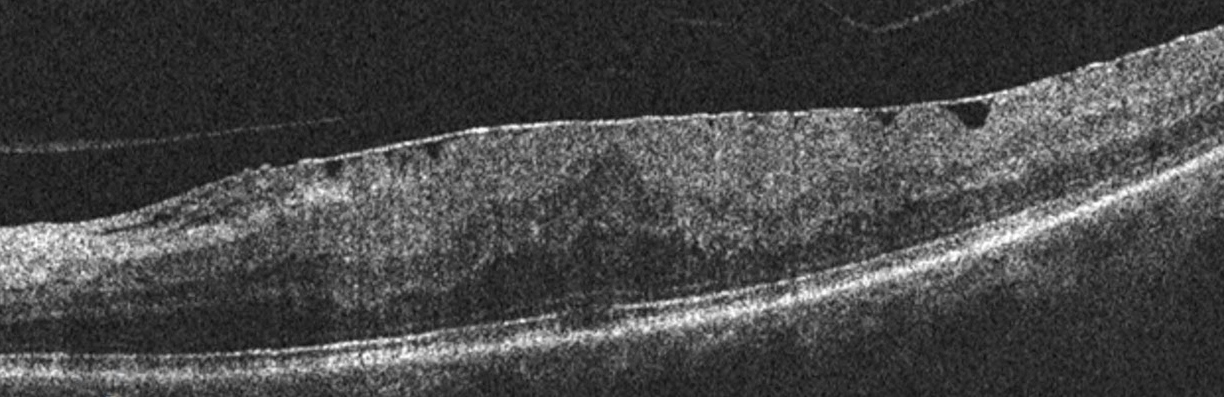
A simple examination from an ophthalmologist or retina specialist is often enough to diagnose a macular pucker or hole. However, additional testing is often useful in diagnosing subtle cases or monitoring eyes for changes. An optical coherence tomography (OCT) scan is a specialized photograph that allows your physician to look for microscopic changes in the contour of the macula. The following figures show an OCT of a normal macula, a macular hole, and a macular pucker. Note that the normal macula has a central dip known as the fovea, shown in Figure 1. In Figure 2, the dip is replaced by a gap which is a macular hole. Finally, Figure 3 shows a macular pucker where the dip is no longer visible. This is because the macular pucker, seen as a thin white line is distorting the normal shape of the macula.
What treatments are available for macular puckers and macular holes?
Macular puckers can be quite mild. For mild cases in patients with minimal symptoms, periodic monitoring may be all that is required. When blurred vision due to a macular pucker begins to affect activities such as driving or reading, treatment in the form of surgery can be considered. Surgery for a macular pucker is known as a vitrectomy. Vitrectomy surgery is usually done under local anesthesia and as an outpatient procedure. During the surgery, fine instruments are used to remove the scar tissue from the surface of the macula. After surgery, patients usually experience an improvement in the blurring and distortion as the eye recovers gradually over a period of months. Some residual waviness can be normal. Vitrectomy is generally very safe although there is a chance of increased cataract growth and a small risk of infection or retinal detachment.
For patients with small macular holes, close monitoring can also be an option since some macular holes can close on their own. For larger holes, there are two options. In select cases where the vitreous gel is actively pulling on the macula, an injection of medication into the eye may cause the gel to release cleanly, allowing the hole to close. In other cases, vitrectomy is recommended. During the surgery, any pulling on the macula is relieved and a gas bubble is placed in the eye to help the hole close. After surgery, patients are asked to look down for a several days to allow the bubble to float up against the hole. Once the body absorbs the bubble, vision is usually significantly improved.
In summary, both macular puckers and holes are common causes of blurry or distorted central vision. If treatment or surgery by a retina specialist is needed, the results are generally quite good and lead to significant restoration of vision.