Corneal Scratches and Abrasions
Call it a scratch, an abrasion or erosion; no matter how you describe it or what the cause, damage to the cornea most always causes pain.
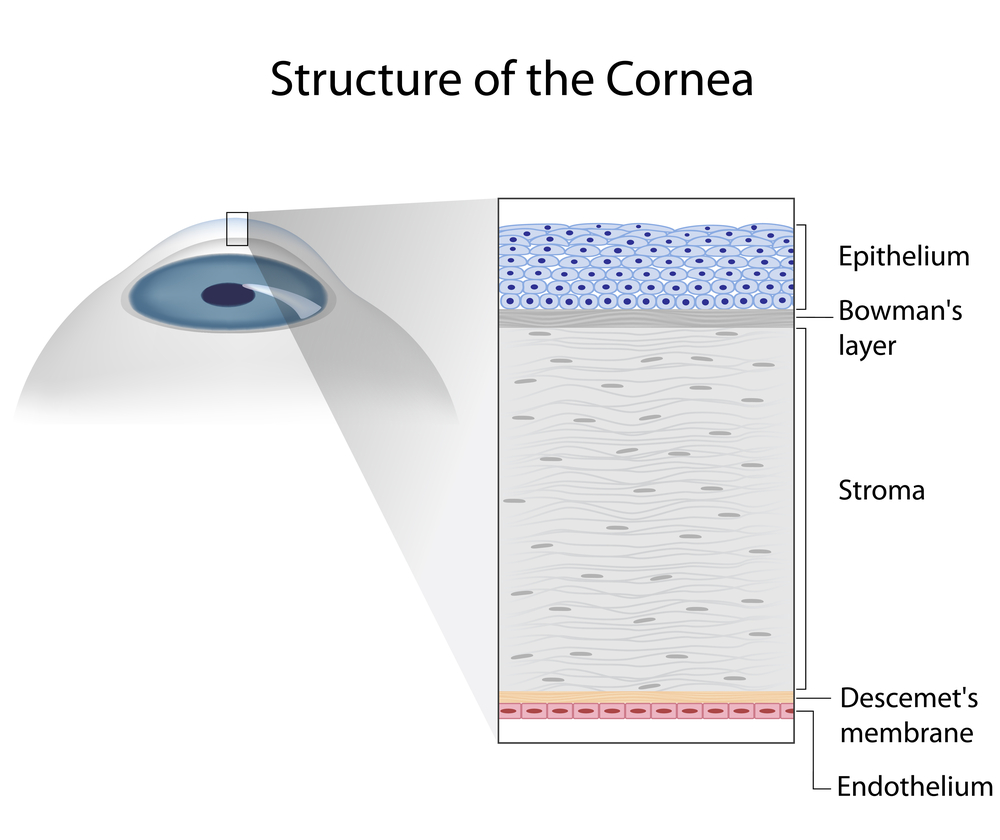
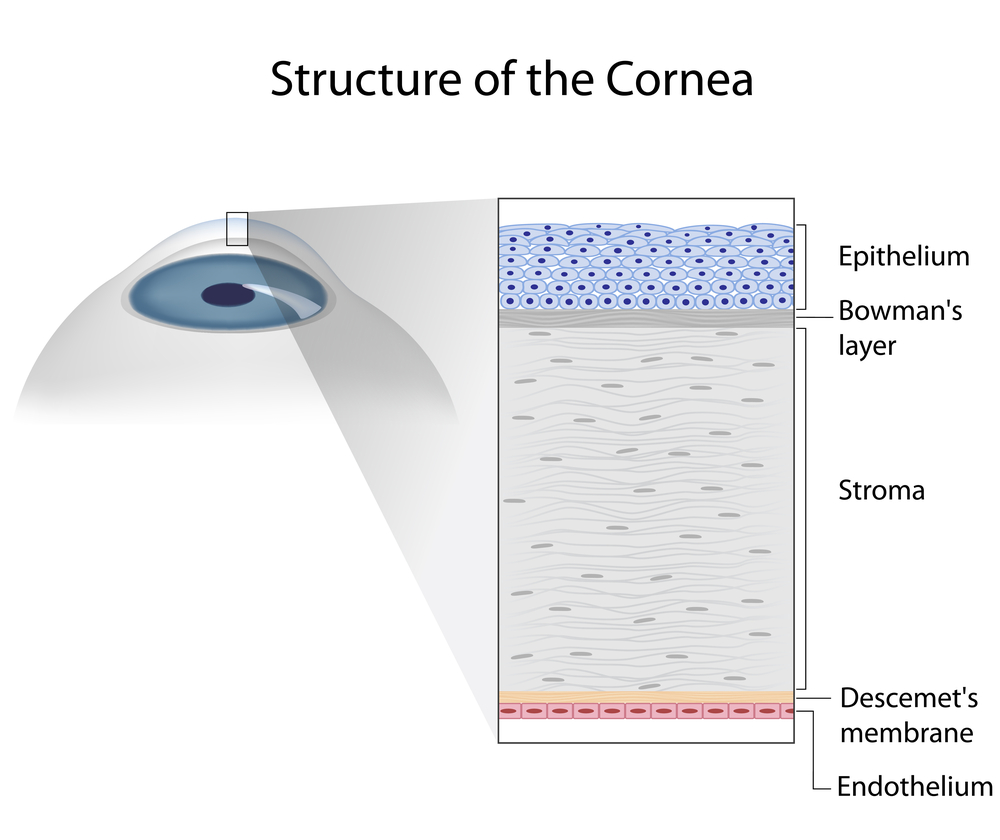
So what exactly is the cornea and why can even a small scratch hurt so much? The cornea is the clear dome at the very the front of the eye. Its primary job is to surface the tears and with them, focus light into the eye. It then passes through the crystalline lens and on to the retina where it is transformed into electrical impulses that are ultimately transformed by the brain into sight.
Because vision is so essential for survival and the cornea so critical to seeing, it is among the most richly innervated and exquisitely sensitive of all tissues. Even the smallest piece of dust that finds its way into the eye and touches the cornea can cause significant discomfort, irritation and copious tearing in an attempt to wash it away. A healthy cornea is transparent and consists of several layers that give the cornea its smooth dome like shape. The outermost layer, the epithelium, is designed to break away to protect the delicate deeper layers if scratched or abraded.
Looking For the Cause
The most common causes of corneal scratches are accidents. Tiny infant fingers and fingernails are a common cause of abrasions in young parents, tree branches are a frequent source of abrasions in hikers and lovers of the outdoors, and makeup brushes are a typical cause in women. Scratches can also be caused by foreign objects that get into the eye and then work their way on to the inside of the upper lid – causing a scratch that occurs with each blink. That’s why its important to carefully investigate the cause of every corneal scratch.
A scratch pr abrasion usually produces near instantaneous pain and tearing as the eye tries to wash away the irritant. Light sensitivity soon follows and can be so intense that the eye can involuntarily shut. This is actually nature’s way of “patching” the eye to facilitate healing.
To confirm you have a scratched cornea, a doctor or other health care professional will often apply a wetted fluorescein strip to the inside lid or white of the eye. Fluorescein is a dye that glows bright green when exposed to black light. The dye is absorbed by damaged areas, clearly showing the area if the scratch or abrasion.
Getting On the Mend
The good news is that most scratches will rapidly heal on their own, especially smaller and more superficial ones. The confocal microscope, a high tech device that provides extreme magnification views of living tissue, has been used to observe corneal healing in real time. The video captures are breathtaking as individual corneal cells can be seen literally stretching over each other to mend and seal the corneal surface.
If an abrasion is larger or deeper it may require patching to help healing. The traditional eye patch applied with tape to keep the eye shut has largely been replaced by the bandage contact lens which is far more comfortable and allows some vision and easier observation during follow up examination. It also allows medication to be applied if needed. Because there is a risk of infection whenever the outer boundaries of the body are breached, topical antibiotics are often used as a precaution in treating scratches of the cornea and ocular surface.
Most commonly the cornea heals quickly and completely, but not always. In rare cases damaged areas of the cornea may not heal fully, leaving the outer layers of the cornea susceptible to coming off again for no apparent reason. This is thought to be more common after scratches caused by organic material such as a tree branch. Called recurrent corneal erosions, they often occur during sleep waking the person with a sudden sharp pain and excessive tearing. There are a variety of treatments for recurrent corneal erosion.
Conclusion
Most people will sooner or later experience a scratched cornea. Most scratches will be minor and will resolve with minimal treatment. However, some can be serious and have significant consequences. The best way to avoid problems is to be aware that they can occur and take measures to protect the eyes in situations where the risk of eye trauma is higher. This includes: wearing safety glasses while working with power tools, or sports where eye contact is possible. This includes cycling and sport shooting.
Be aware of active infants with little fingers that seem to have a magnetic attraction of their parents eyes. If you use eye makeup, leave enough time to properly apply it without rushing and potentially scratching your cornea in the process.
Finally, if you experience a scratched cornea and the pain doesn’t rapidly abate, see an eyecare specialist. Urgent care centers are fine for most things, but when it comes to the eyes finding a knowledgeable eye care professional is wise.
2/10/15
 Arthur B. Epstein, OD, FAAO
Arthur B. Epstein, OD, FAAO
co-founder of Phoenix Eye Care
and the Dry Eye Center of Arizona
Fellow of the American Academy of Optometry
American Board of Certification in Medical Optometry
Chief Medical Editor of Optometric Physician™