Meet Tom Sullivan – DEF’s Ambassador of Vision
Meet Tom Sullivan – DEF’s Ambassador of Vision
Over the last 40 years, I’ve been committed to working on behalf of blind children and their families. My involvement has spanned the entire gamut of participation – from direct involvement in the classroom and counseling parents to hosting organized 10K races and celebrity golf tournaments that carried my name. In that time, my wife and I raised just over $8 million thanks to the generosity of so many people. Though my commitment to this cause has not changed, I’ve chosen to take on a new challenge that has in every way re-energized my passion.
I’ve recently become the Ambassador of Vision for the Discovery Eye Foundation (DEF), a remarkable organization that funds cutting edge research that I believe someday will eliminate many forms of blindness. The principle reason for my enthusiastic commitment is largely due to the fact that DEF directly funds researchers and avoids institutional restrictions.
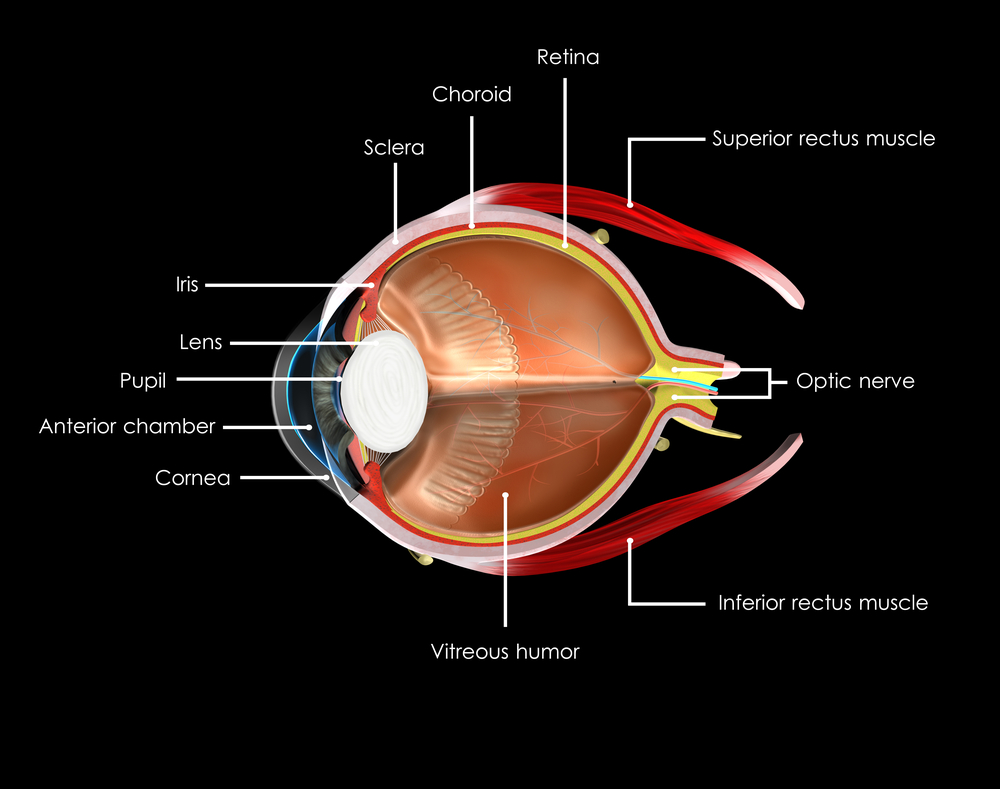
As of this blog, DEF is engaged in ongoing efforts to understand 5 main eye diseases – Retinitis Pigmentosa, Macular Degeneration, Keratoconus, Diabetic Retinopathy, and Glaucoma. I can honestly tell you that breakthroughs are not only on the horizon, but in many cases they are imminent. Over the weeks and months I’ll be telling you much more, specifically about our individual research projects.
Any help you may choose to give on behalf of people struggling with vision loss will be deeply appreciated. I look forward to having many of you join my fight for sight. Your help can make a difference! Click here to donate.
 Tom Sullivan
Tom Sullivan
DEF’s Ambassador of Vision
sullivanvision.com