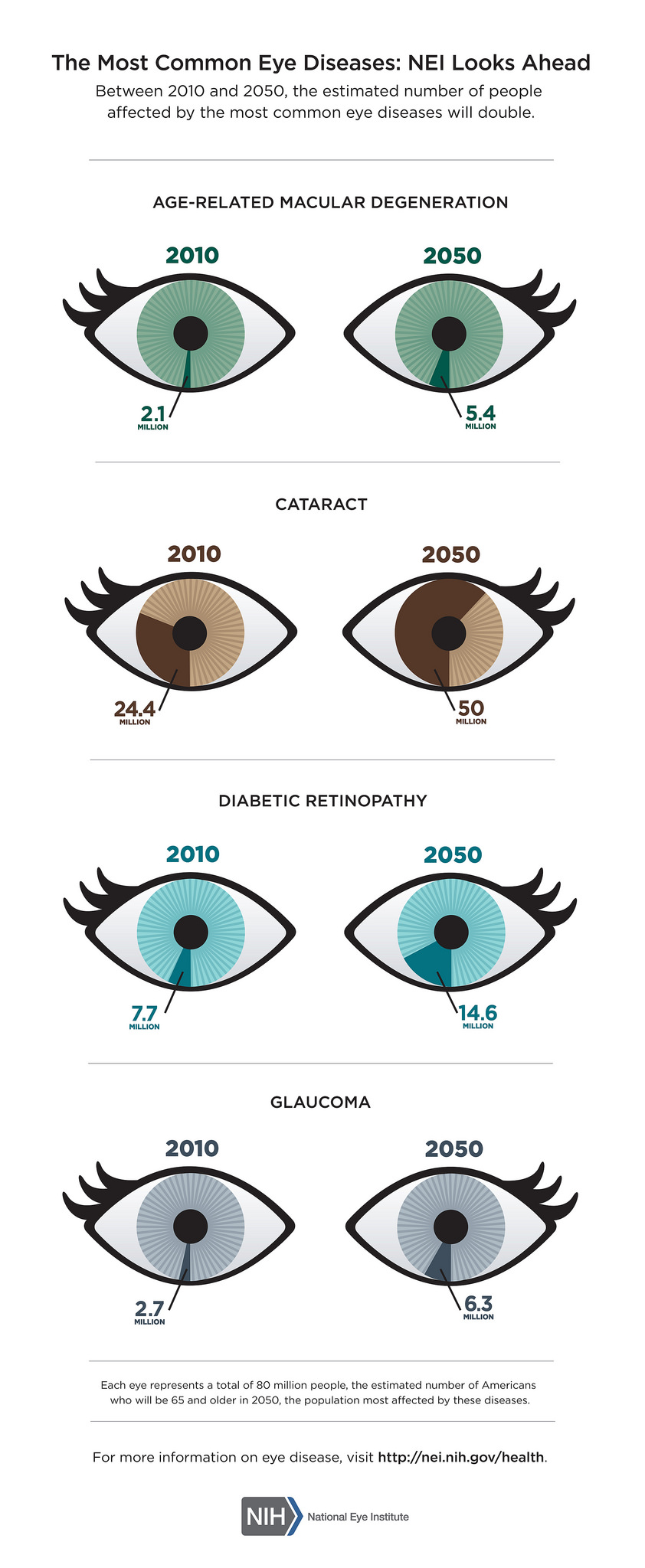
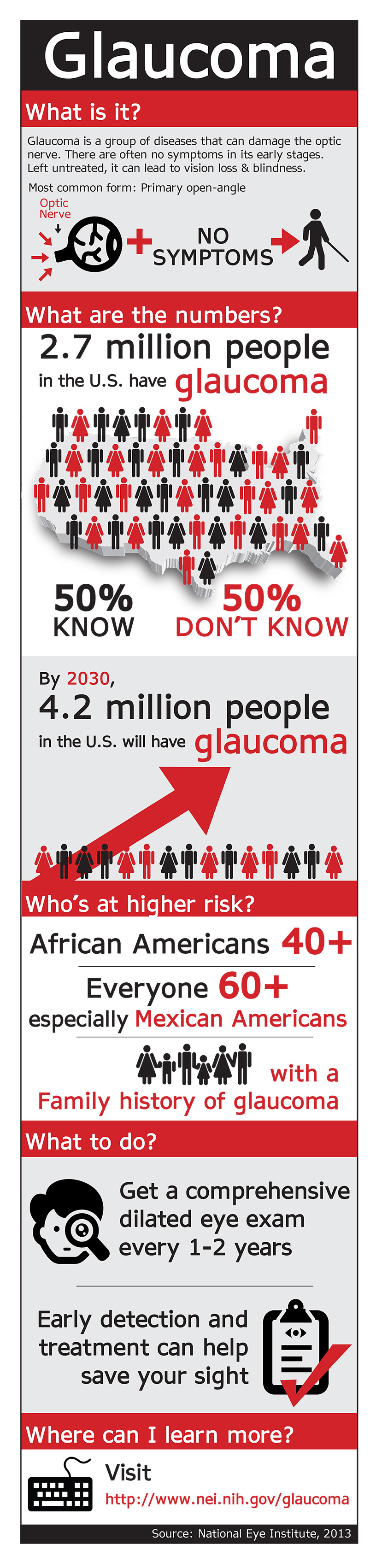
Low vision in aging adults varies as do the occupational therapy techniques that might help older adults in becoming more independent. Mr. P has glaucoma resulting in a narrowed field of view. He is light sensitive, and keeps his blinds closed, darkening the house. He is responsible for doing his laundry, yet his washer and dryer are in the basement, causing a safety concern. Mrs. K has macular degeneration with 20/400 visual acuity. She has severely reduced contrast sensitivity, and can no longer drive or recognize faces easily. She no longer gets to the senior center for regular exercise sessions, which is concerning to her and her OT. Ms. T was diagnosed with diabetic retinopathy. She has struggled for years to accurately see her glucometer and insulin. She has recently developed peripheral neuropathy, leading to wheelchair dependency. Each of these patients is likely to leave their home less often because of their low vision, eventually leading to a decline in lower extremity weakness, balance, endurance and confidence. The fear of falling leads to more isolation, which can cause even more lower extremity weakness, problems with balance, decreased endurance, and even depression. The irony is that this cycle, which began with caution and a fear of falling, lends itself to exactly that. . .a fall.
Why are low-vision aging adults at higher risk for falls?
According to the CDC, “Each year, millions of older people-those 65 and older-fall. In fact, one out of three older people fall each year, but less than half tell their doctor. Falling once doubles your chances of falling again.” The typical aging adult with low vision faces challenges that others do not. Difficulty seeing details combined with reduced contrast sensitivity leads to a decline in mobility and socialization.

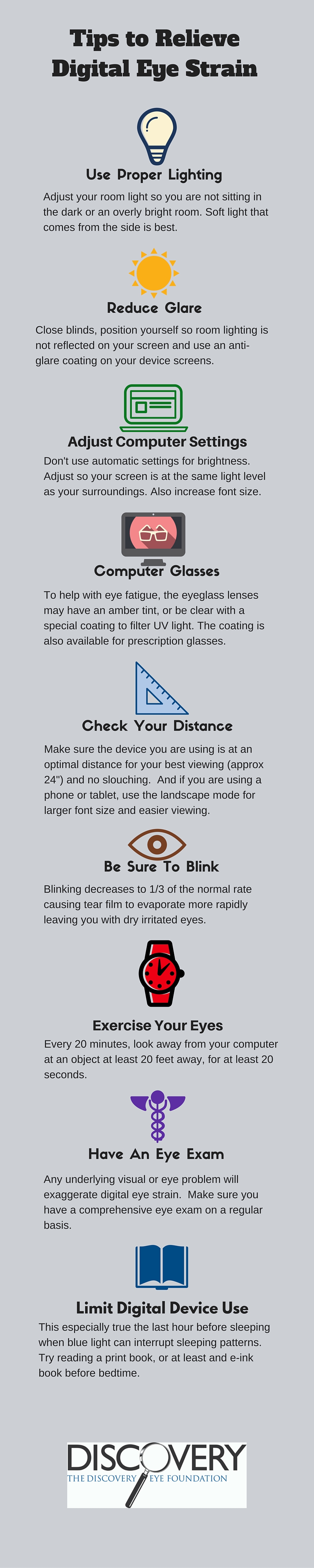
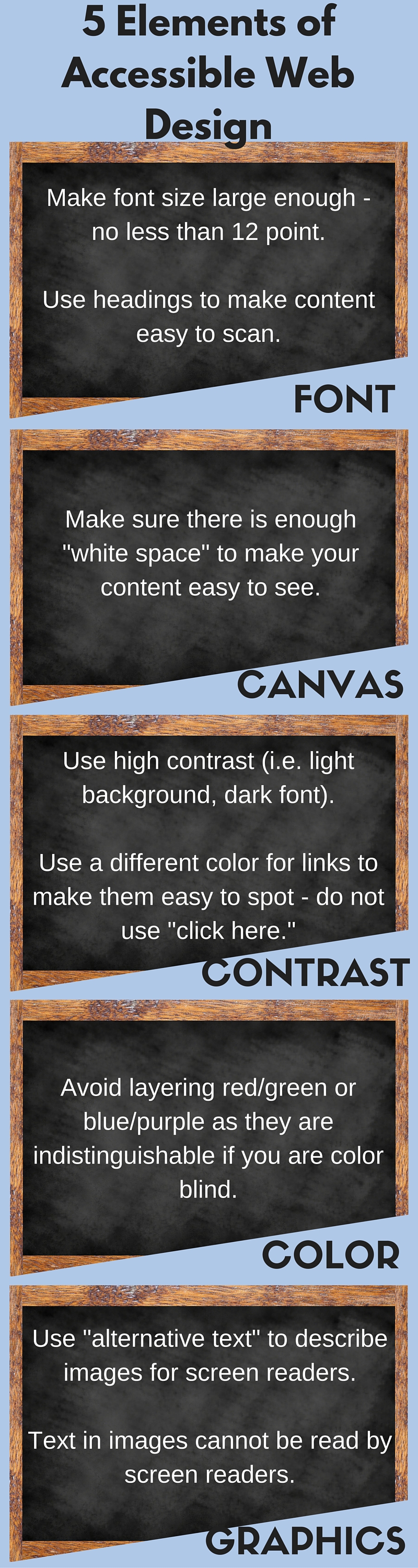
So how do we help older adults with low vision lower their risk for falling? When considering safety within the home, persons with low vision must make it a priority to add lighting & contrast whenever possible. Consider all rooms of the house, including entrances, hallways and stairways.
- Placement of night lights in hallways, stairway, etc.
- Keep flashlights in accessible places throughout the home where night lights are not possible.
- Instead of closing blinds, keep them open & wear appropriate colored filters to manage glare/light sensitivity.
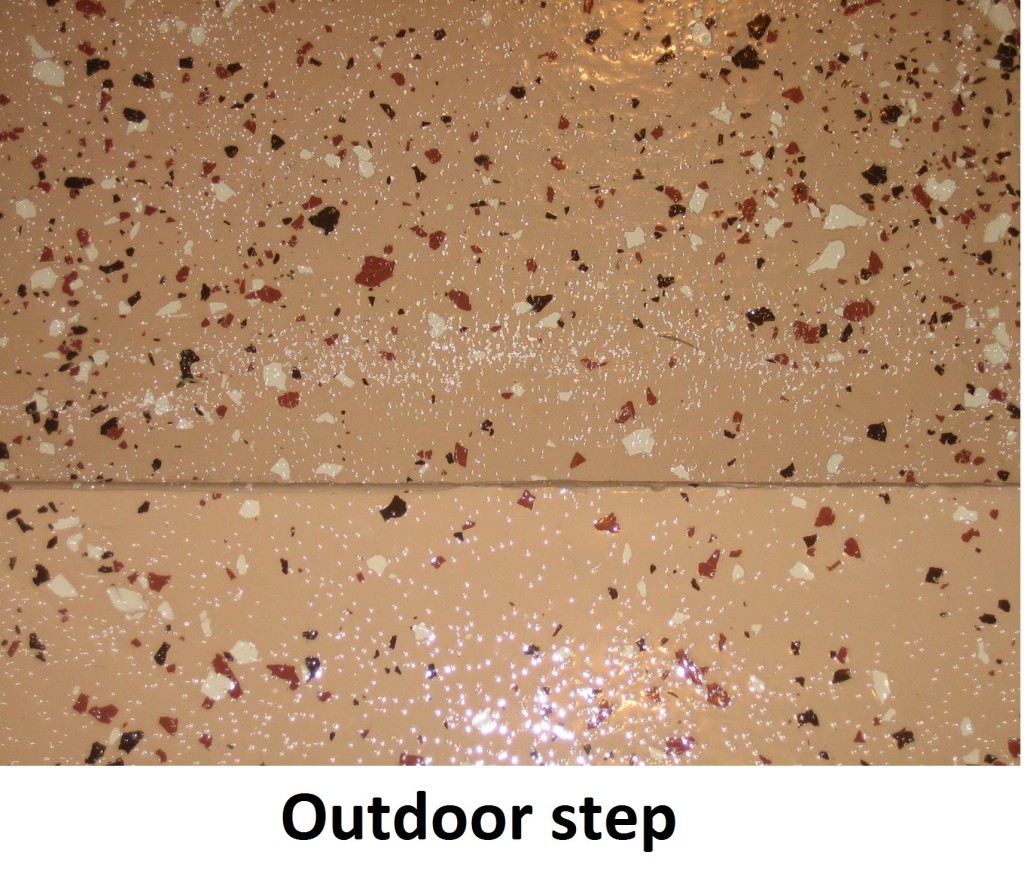
- Small battery operated stick-on lights or rope lighting is inexpensive, and easy to place on steps to light up a stairwell.
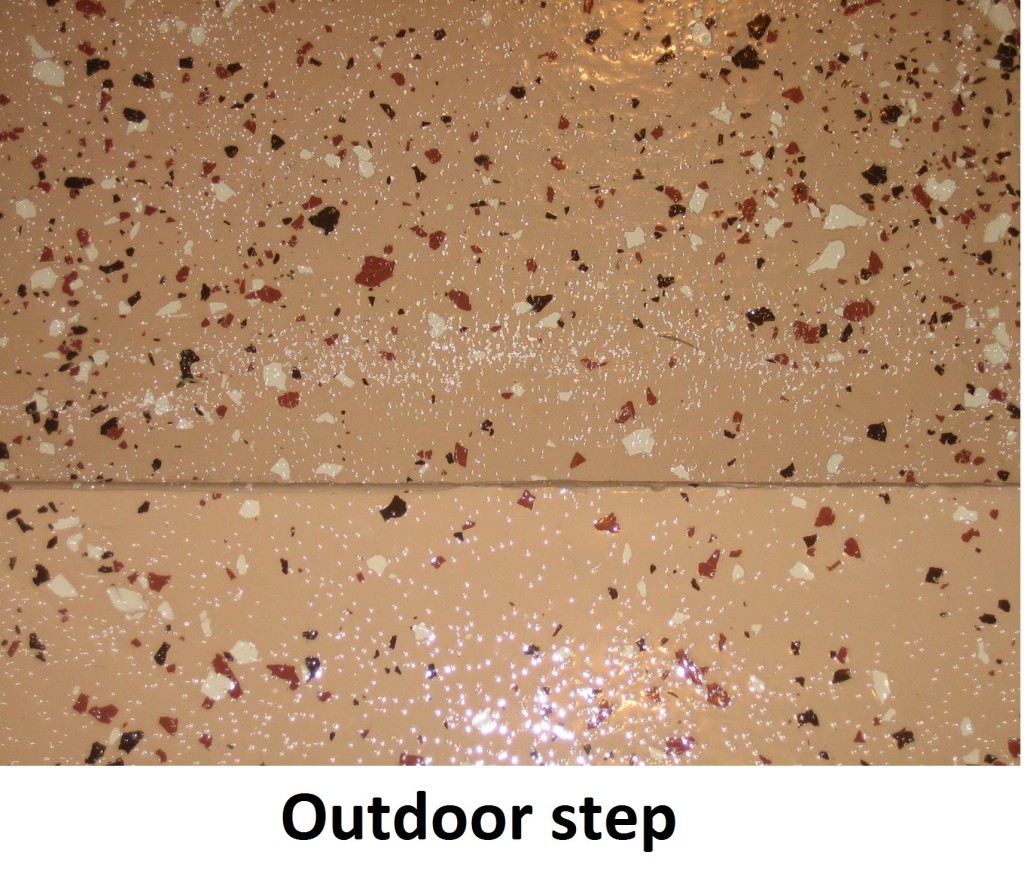
- Line edge of steps, or stairway railing with brightly colored duct tape to increase visibility.
- Make sure grab bars, tub benches, shower chair are high contrast, to be most visible.
- Remove throw rugs, with the exception of those providing function, such as the one at the entrance and bathtub. Their purpose is for providing dry shoes and feet, but they should have a non-skid back and a high contrast color to “stand out.”
- Reduce clutter in rooms to increase safety by removing items from floors, walkways and stairwells.
- Consider investing in a Medical Alert System to provide added piece of mind, confidence, especially when living alone.
Persons with low vision can decrease their frequency of falls by staying social and walking in the community. Unfortunately, many low vision adults become more house bound when they can no longer drive. Locating sources of alternative transportation may be helpful. Seeing faces is difficult, making socializing a challenge, which can lead to depression. The following recommendations take into consideration the challenges of not seeing details or across the visual field normally, while improving lower body strength, endurance, coordination, confidence, and hopefully reducing the risk of a fall.
- Encourage regular trips to the grocery stores and the mall to keep physically fit. Malls are safe environments to walk around because of wide, straight hallways. Use magnifiers to see price tag/label details, or take advantage of personal shoppers who assist with locating items.
- Participate in regularly scheduled exercise sessions (videos, groups, etc). Sit/stand in the front row, ask instructor to provide clear verbal instruction, instead of only demonstration. Consider hiring a personal trainer in order to get 1:1 instructions for how to use exercise equipment. If watching a video, move closer to your largest TV screen. Home exercise equipment can be labeled with high contrast markings to increase visibility of its details.
- Consider joining a senior center in the community. Some have low vision support groups.
- Access driving alternatives, such as the Smart Bus, Senior Centers, Local Volunteer or Church groups. Consider using money previously spent for a car and its expenses to hire a private driver.
- Use appropriate colored filters in bright outside conditions or darker inside environments (i.e. Amber outside in the sun; Yellow inside a dark restaurant or outside with overcast weather).
- Consider using a walker or support cane when walking longer distances in the community or neighborhood. Many individuals decline using an assistive device, not realizing how active and fit it can make them. Rolling walkers are even available with seats, allowing for rest breaks wherever necessary.
While the fear of falling is great amongst all seniors, those with low vision need to consider adding strategies that specifically benefit them. Making changes within the home may be as simple as improving lighting and contrast. Remaining physically fit outside of the home may be done with shopping or exercise equipment, but either way staying active will improve confidence, the fear of falling, and hopefully decrease the chance of a fall. If you are unsure of what approach is best for you, consult with your ophthalmologist about scheduling a low vision eye exam and occupational therapy.
Reference:
Centers for Disease Control and Prevention, National Center for Injury Prevention and Control-CDC 24/7: Saving Lives, Protecting People
12/3/15
 Annette M. Babinski, OTR/L CLVT
Annette M. Babinski, OTR/L CLVT
Henry Ford Health System
Vision Rehabilitation Center
 Michelle Buck, MS, OTR/L CLVT
Michelle Buck, MS, OTR/L CLVT
Henry Ford Health System
Vision Rehabilitation Center
 Susan DeRemer, CFRE
Susan DeRemer, CFRE