Medical research funding from the US government, the medical device and pharmaceutical industries, biotech and foundations has dropped 0.8% per year, every year from 2007 to 2012. Even with the economic recovery, the funding of eye research from the NIH in 2014 decreased by 17% from 2012.
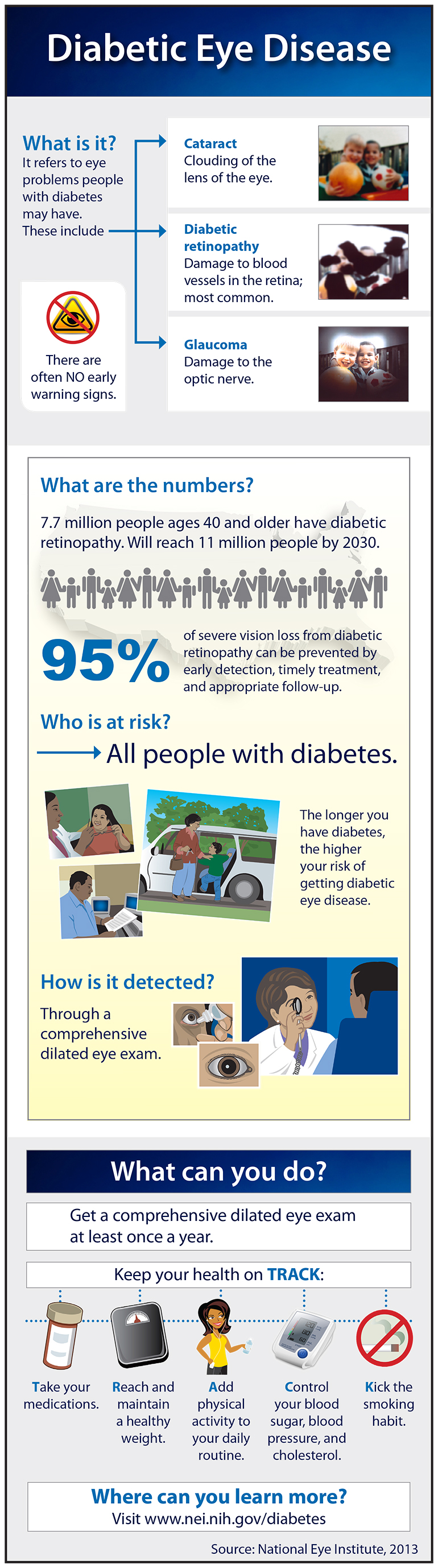
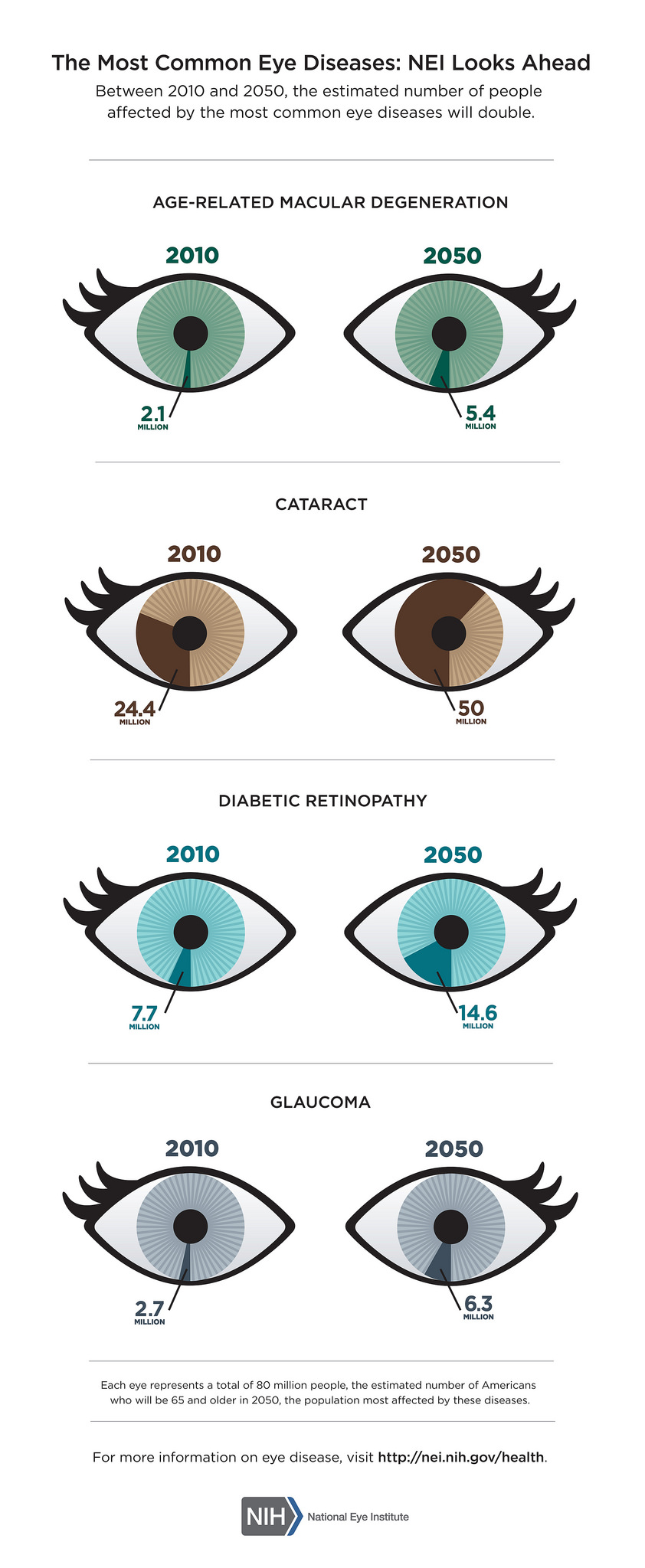
What makes this particularly disturbing is that the need for eye research is more important now than ever, as demonstrated by the infographic below.
Giving For Eye Research
The eye diseases in the above graphic are related to aging. The number of people being affected is more than doubling for each eye diseases, except for diabetic retinopathy which will increase by 47%, by 2050.
While we are more health conscious than in previous years, knowing the importance of exercise, healthy eating and not smoking, the US population is aging.
Aging baby boomers, the largest population group in US history, are creating a dramatic shift in the age composition of the U.S. population. It is projected that the entire senior population, including the pre-boomer silent generation, will reach 71.4 million people by 2029. This means that those people 65 and older will make up about 20%of the US population by 2029, up from almost 14% in 2012.
We need your help to find treatments and cures for these sight-threatening eye diseases.
December 1st will be the fourth year of #GivingTuesday. It is a global day of giving using combined power of social media and collaboration. Always the Tuesday following Thanksgiving, it has become as widely recognized as Black Friday and Cyber Monday and kicks off the philanthropic season, when many focus on their holiday and end-of-year giving.
We are asking that you support eye research through the Discovery Eye Foundation this philanthropic season with a gift on #GivingTuesday. It is easy to do; you can do it from the comfort of your home – just click here.
Also share this post with family and friends so they can also give the gift of sight this holiday season.
Thank you for reading our blog and for your support.
11/24/15
 Susan DeRemer, CFRE
Susan DeRemer, CFRE
Vice President of Development
Discovery Eye Foundation