How many times have we heard: “This field has been thoroughly studied, and we know all there is to know; there is no reason to continue investigating, because there is nothing more to find out on the subject”? This has been the attitude of some researchers with respect to the importance of mitochondria and diseases. For more than 50 years, we have known that mitochondria, which are the “batteries” of the cell, are critical for energy production. But many believed they did not have other major roles in the health of the cell, so when it came to developing drugs against diseases, mitochondria were overlooked.
That idea has now been turned on its head.
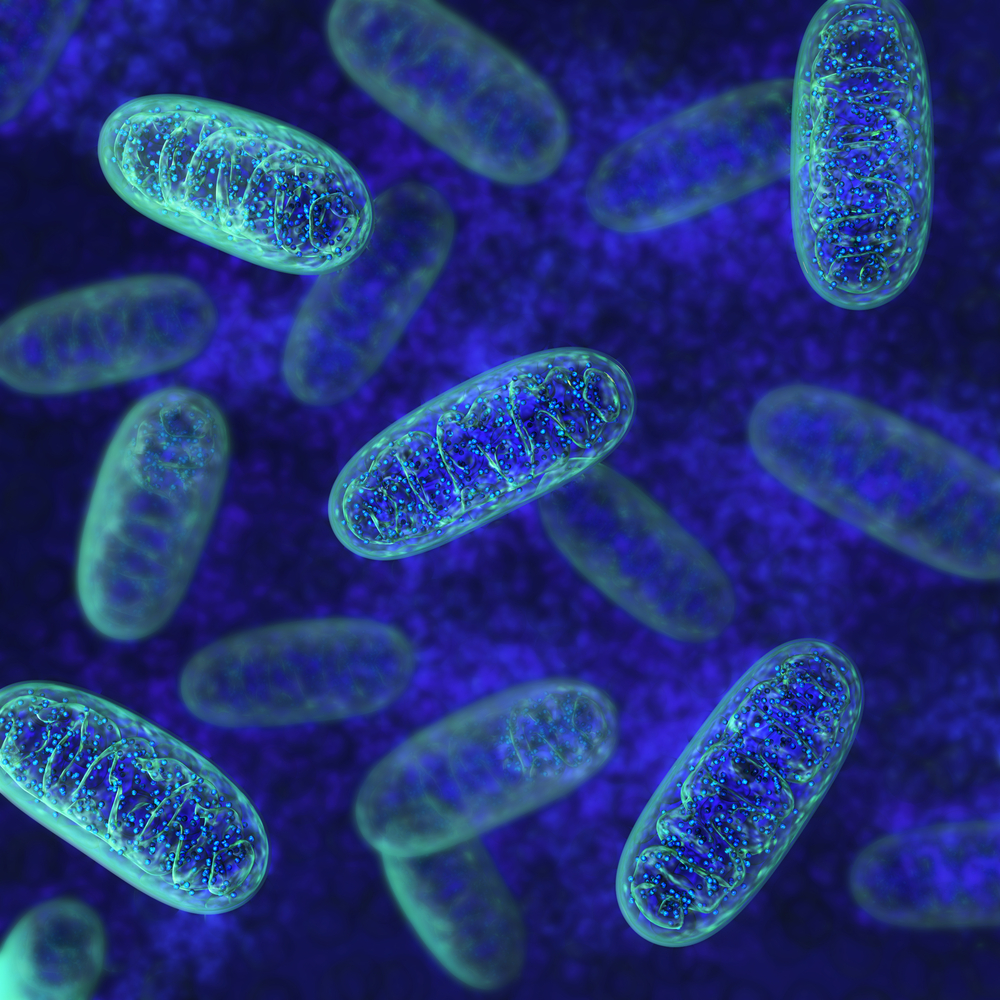
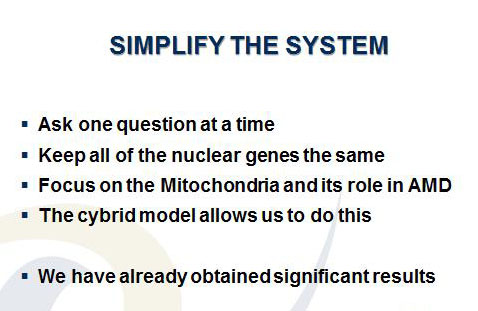
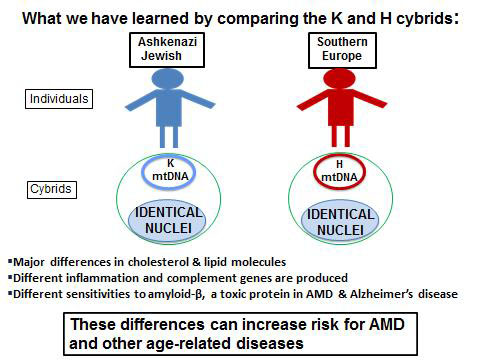
Led by Discovery Eye Foundation (DEF) Research Director Dr. Cristina Kenney, the Mitochondria Research Group believed that, to really discover something new, you have to look in novel areas. This group has done just that. Using the transmitochondrial cybrid model, which are cell lines with identical nuclei, but with each line containing mitochondria from a different person, they have shown that the mitochondria have major regulation powers over cell behavior and expression of disease-related pathways. This is significant, because the mitochondria then become a target for therapies to combat diseases.
Kenney’s group is investigating various drugs and substances that will keep the mitochondria healthy and, ultimately, improve the health of the retinal cells in age-related macular degeneration (AMD). But it does not stop there. This same approach to developing mitochondria-targeting drugs is being pursued for drugs to treat Parkinson’s disease, Alzheimer’s disease, leukemia, various cancers, heart failure, thrombosis, stroke, diabetic retinopathy, Leber hereditary optic neuropathy, and even liver toxicity from acetaminophen.
The continued support from DEF, especially in the early stages of the mitochondria research, has fostered a new area to be opened up, specifically for AMD and diabetic retinopathy. In turn, this has allowed new collaborations among Kenney and researchers from the eye field, and laboratories studying the brain and neurodegeneration, cardiology, cancer therapies and methods to reduce side effects from cancer drugs. Kenney’s discoveries using cybrids have revolutionized the field of mitochondrial research, showing that mitochondria have wide-ranging biological effects never imagined and opening up the field of mitochondrial therapy to careful investigation.
You can help make a difference by supporting DEF’s sight saving research. Help our researchers advance AMD research by donating today!
 Lauren Hauptman
Lauren Hauptman
Lauren Hauptman Ink



 The National Eye Institute has recommended that people who are high-risk for developing AMD eat diets rich in green leafy vegetables, whole fruits, any type of nuts and omega 3 fatty acids. Many of these foods have anti-oxidant properties that help to “turn off” genes involved with inflammation, an important factor of retinal diseases. Salmon, mackerel and sardines have the highest levels of omega-3 fatty acids. An analysis that combined the data from 9 different studies showed that fish intake at least twice a week was associated with reduced risk of early and late AMD. Other studies show that Omega-3 fatty acids improve mitochondrial function, decreases production of reactive oxygen species (free radicals that damage cells) and leads to less fat accumulation in the body. The green leafy vegetables contain important protective macular pigments (carotenoids) called lutein and zeaxanthin that reduce the risk of AMD by 43%. High levels of lipid or fat deposits in the body (obesity) can “soak-up” the lutein and zeaxanthin so that they are not available to protect the retina.
The National Eye Institute has recommended that people who are high-risk for developing AMD eat diets rich in green leafy vegetables, whole fruits, any type of nuts and omega 3 fatty acids. Many of these foods have anti-oxidant properties that help to “turn off” genes involved with inflammation, an important factor of retinal diseases. Salmon, mackerel and sardines have the highest levels of omega-3 fatty acids. An analysis that combined the data from 9 different studies showed that fish intake at least twice a week was associated with reduced risk of early and late AMD. Other studies show that Omega-3 fatty acids improve mitochondrial function, decreases production of reactive oxygen species (free radicals that damage cells) and leads to less fat accumulation in the body. The green leafy vegetables contain important protective macular pigments (carotenoids) called lutein and zeaxanthin that reduce the risk of AMD by 43%. High levels of lipid or fat deposits in the body (obesity) can “soak-up” the lutein and zeaxanthin so that they are not available to protect the retina.