 The other day my daughter Blythe asked me which Christmas I consider to be my favorite. I had to think a minute, because as a family, the Sullivan’s have had some great ones. I was about to say the first time you and your brother Tom were old enough to really get into Santa, being absolutely sure that the fat man brought your presents right down the chimney. I was about to say that, and then I remembered.
The other day my daughter Blythe asked me which Christmas I consider to be my favorite. I had to think a minute, because as a family, the Sullivan’s have had some great ones. I was about to say the first time you and your brother Tom were old enough to really get into Santa, being absolutely sure that the fat man brought your presents right down the chimney. I was about to say that, and then I remembered.
The greatest Christmas I ever enjoyed was a ski trip in Winter Park,  Colorado, when our children were teenagers and our friend, the marvelous Betty White, joined us for a Christmas Eve sleigh ride none of us will ever forget. The night was perfect. It had snowed earlier that day, and the air had a feeling of Christmas that you could almost taste. Oh, sure, it was cold, but we were bundled up under tons of blankets as two beautiful Clydesdale horses with bells jingling took us through the woods to a magical barn where dinner would be served and carols sung.
Colorado, when our children were teenagers and our friend, the marvelous Betty White, joined us for a Christmas Eve sleigh ride none of us will ever forget. The night was perfect. It had snowed earlier that day, and the air had a feeling of Christmas that you could almost taste. Oh, sure, it was cold, but we were bundled up under tons of blankets as two beautiful Clydesdale horses with bells jingling took us through the woods to a magical barn where dinner would be served and carols sung.
It was on the way home that my Christmas was made complete. We had stopped to let the horses breathe, and everyone was quiet, just allowing the feeling of togetherness envelope us in that special night. It was Betty who broke the silence.
“Tom,” she said almost to herself, “I wish I may, I wish I might, let you see the stars tonight. I feel like we could almost reach up and touch them. That’s how bright and close they are. I guess when you’re this high in the Rocky Mountains, it just feels like they’re right here.”
I could hear how much my friend wanted me to see such a heavenly display, but we both knew that could never happen. I have no complaint about being blind, no one could have a better life, but I would be lying if I didn’t admit at this holiday season that I’d love to be able to take it all in, all the special sights of Christmas.
Every day in laboratories around this country, researchers are working to solve the multiple eye diseases that make it impossible for millions of people to see the joys of Christmas. At this holiday season, my best gift would be that all of us donate to the Discovery Eye Foundation with its goal to preserve vision and eradicate blindness around the world. During this season of giving, may your hearts be light and your sight be bright.
Merry Christmas!
 Tom Sullivan
Tom Sullivan
DEF’s Ambassador of Vision
sullivanvision.com


 Harsh weather conditions can reduce the natural moisture in your eyes and the irritation usually results in a burning or itching sensation that often leads to rubbing or scratching your eyes which can worsen the symptoms. Sometimes it feels like there is a foreign object in your eye and for some, dry eyes can even cause excessive tearing, as your eyes try to overcompensate for their lack of protective tears. Prolonged, untreated dry eyes can lead to blurred vision as well. Between the harsh winter winds outside and the dry heat radiating inside, our eyes are very quickly irritated and dried in the winter months. The result is itchy, dry eyes that may cause pain, blurred vision, a burning sensation, or even watery vision as our eyes try to compensate for the dryness.
Harsh weather conditions can reduce the natural moisture in your eyes and the irritation usually results in a burning or itching sensation that often leads to rubbing or scratching your eyes which can worsen the symptoms. Sometimes it feels like there is a foreign object in your eye and for some, dry eyes can even cause excessive tearing, as your eyes try to overcompensate for their lack of protective tears. Prolonged, untreated dry eyes can lead to blurred vision as well. Between the harsh winter winds outside and the dry heat radiating inside, our eyes are very quickly irritated and dried in the winter months. The result is itchy, dry eyes that may cause pain, blurred vision, a burning sensation, or even watery vision as our eyes try to compensate for the dryness. I can only imagine my wife’s beautiful face. Oh sure, I’ve touched it and kissed it many times. I’ve felt the lines with the tips of my fingers, tracing our lives together, and I’ve heard her smile. I understand that’s not really seeing it. It’s not seeing her eyes as they sparkle with something funny I said; or, when she looks at me with love reserved only for those who are truly in love.
I can only imagine my wife’s beautiful face. Oh sure, I’ve touched it and kissed it many times. I’ve felt the lines with the tips of my fingers, tracing our lives together, and I’ve heard her smile. I understand that’s not really seeing it. It’s not seeing her eyes as they sparkle with something funny I said; or, when she looks at me with love reserved only for those who are truly in love.
 Costume Contact Lenses such as cat eyes or zombie may make your Halloween costume a bit more frightful although wearing those lenses without a prescription can be more terrifying, as it could result in vision loss or even blindness.
Costume Contact Lenses such as cat eyes or zombie may make your Halloween costume a bit more frightful although wearing those lenses without a prescription can be more terrifying, as it could result in vision loss or even blindness.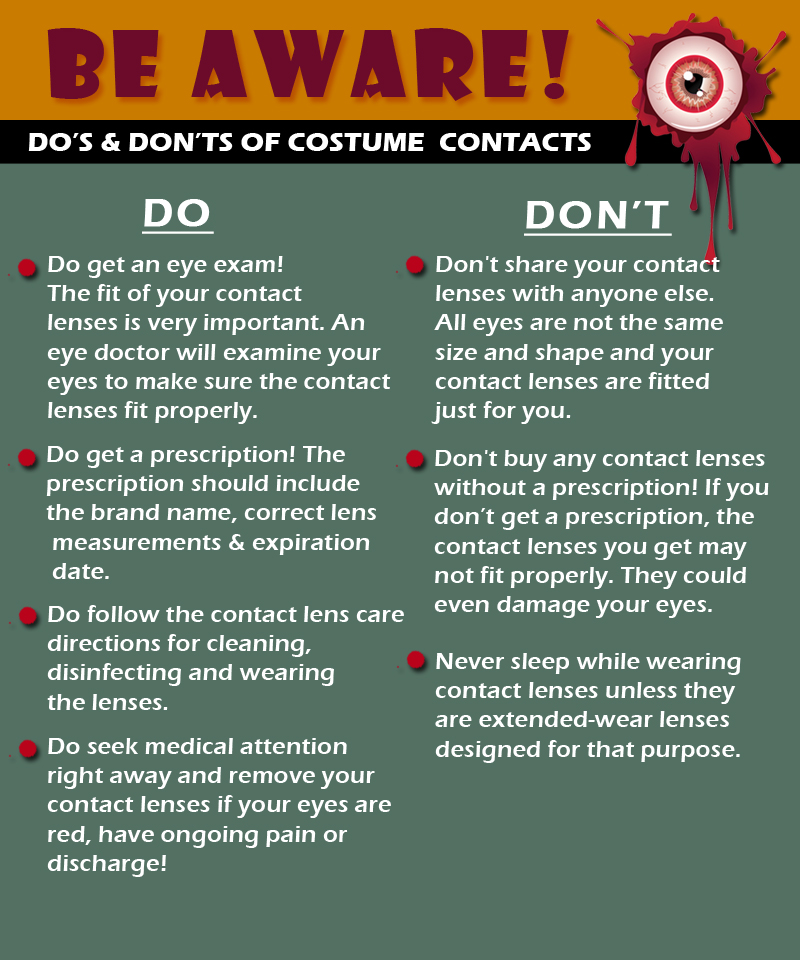
 I could hear Charlie rubbing his wife’s shoulders and telling her that everything would be alright. But, Rose kept saying “I know we’ll have to sell the house and move into something smaller, and I am going to be blind Charlie. Blind.”
I could hear Charlie rubbing his wife’s shoulders and telling her that everything would be alright. But, Rose kept saying “I know we’ll have to sell the house and move into something smaller, and I am going to be blind Charlie. Blind.” Today, people are living longer than ever before so it’s important to be proactive and take responsibility for your health as you age.
Today, people are living longer than ever before so it’s important to be proactive and take responsibility for your health as you age. 
 Maintain a healthy weight. Being overweight increases your risk for diabetes. By exercising regularly, you can help keep your body healthy and prevent vision loss.
Maintain a healthy weight. Being overweight increases your risk for diabetes. By exercising regularly, you can help keep your body healthy and prevent vision loss.  Don’t smoke. Smoking increases your risk for age-related macular degeneration, cataract, and other eye diseases and conditions that can damage the optic nerve.
Don’t smoke. Smoking increases your risk for age-related macular degeneration, cataract, and other eye diseases and conditions that can damage the optic nerve. Wear protective eyewear when outdoors. Protecting your eyes from the sun’s ultraviolet rays when you are outdoors is vital for your eye health. Wearing sunglasses that block 99 to 100 percent of both UV-A and UV-B radiation.
Wear protective eyewear when outdoors. Protecting your eyes from the sun’s ultraviolet rays when you are outdoors is vital for your eye health. Wearing sunglasses that block 99 to 100 percent of both UV-A and UV-B radiation. Know your family history. Talk to your family members about their eye health history. It’s important to know if anyone has been diagnosed with a disease or condition since many are hereditary, such as glaucoma, macular degeneration, and diabetes . This will help determine if you are at higher risk for developing an eye disease or condition.
Know your family history. Talk to your family members about their eye health history. It’s important to know if anyone has been diagnosed with a disease or condition since many are hereditary, such as glaucoma, macular degeneration, and diabetes . This will help determine if you are at higher risk for developing an eye disease or condition. Consider a multivitamin. Vitamins C, E and the mineral zinc have been shown to promote eye health. Vitamins with Lutein and Zeaxanthin have been known to help patients with moderate to severe age-related macular degeneration.
Consider a multivitamin. Vitamins C, E and the mineral zinc have been shown to promote eye health. Vitamins with Lutein and Zeaxanthin have been known to help patients with moderate to severe age-related macular degeneration. Give your eyes a rest. If you spend a lot of time at the computer or focusing at any one distance, you sometimes forget to blink, resulting in dryness and eye fatigue. Every 20 minutes, look away about 20 feet in front of you for 20 seconds. This can help reduce eyestrain. Consider using a lubricant eye drop during long periods of intense eye use and rest your eyes for 5 minutes.
Give your eyes a rest. If you spend a lot of time at the computer or focusing at any one distance, you sometimes forget to blink, resulting in dryness and eye fatigue. Every 20 minutes, look away about 20 feet in front of you for 20 seconds. This can help reduce eyestrain. Consider using a lubricant eye drop during long periods of intense eye use and rest your eyes for 5 minutes. Summer time is officially here and everyone enjoys a dip in a nice, cool pool during the summer months. While swimming is a great form of exercise and a relaxing way to cool down, the water can be hard on your eyes.
Summer time is officially here and everyone enjoys a dip in a nice, cool pool during the summer months. While swimming is a great form of exercise and a relaxing way to cool down, the water can be hard on your eyes. Wear Goggles – Wear a pair of swim goggles every time you swim. Goggles keep pool chemicals out of your eyes.
Wear Goggles – Wear a pair of swim goggles every time you swim. Goggles keep pool chemicals out of your eyes. Wash Your Eyes – Immediately after swimming, splash your closed eyes with fresh tap water. This washes chlorine and other chemicals off your eyelids and eyelashes.
Wash Your Eyes – Immediately after swimming, splash your closed eyes with fresh tap water. This washes chlorine and other chemicals off your eyelids and eyelashes. Use Eye Drops – Use over-the-counter lubricating eye drops before and after swimming to keep the tear film balanced and eyes comfortable.
Use Eye Drops – Use over-the-counter lubricating eye drops before and after swimming to keep the tear film balanced and eyes comfortable. Stay Hydrated – Don’t forget to drink plenty of water. Staying well hydrated is an important part of keeping your eyes moist and comfortable.
Stay Hydrated – Don’t forget to drink plenty of water. Staying well hydrated is an important part of keeping your eyes moist and comfortable.

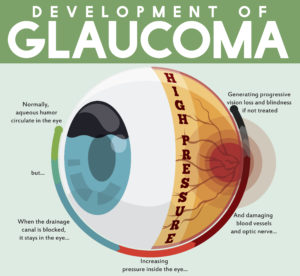 tic nerve, a part of the central nervous system that carries visual information from the eye to the brain.
tic nerve, a part of the central nervous system that carries visual information from the eye to the brain. Summer is almost over and it’s back to school season. As parents, many of us are busy ensuring our kids are ready and prepared for the new year; worrying about school supplies, new clothes, and new haircuts. There is always a long list of things to do before school starts. But something that often gets overlooked is getting your child’s eyes examined annually.
Summer is almost over and it’s back to school season. As parents, many of us are busy ensuring our kids are ready and prepared for the new year; worrying about school supplies, new clothes, and new haircuts. There is always a long list of things to do before school starts. But something that often gets overlooked is getting your child’s eyes examined annually.