In Discovery Eye Foundation’s spring e-newlsetter there was an article entitled Surgery for the Surgeon, where a leading ophthalmologist talks about convincing himself to have cataract surgery. That eye doctor was Dr. Nesburn, who was willing to share with us his family’s long tradition of saving vision.
Brainwashed by Medicine
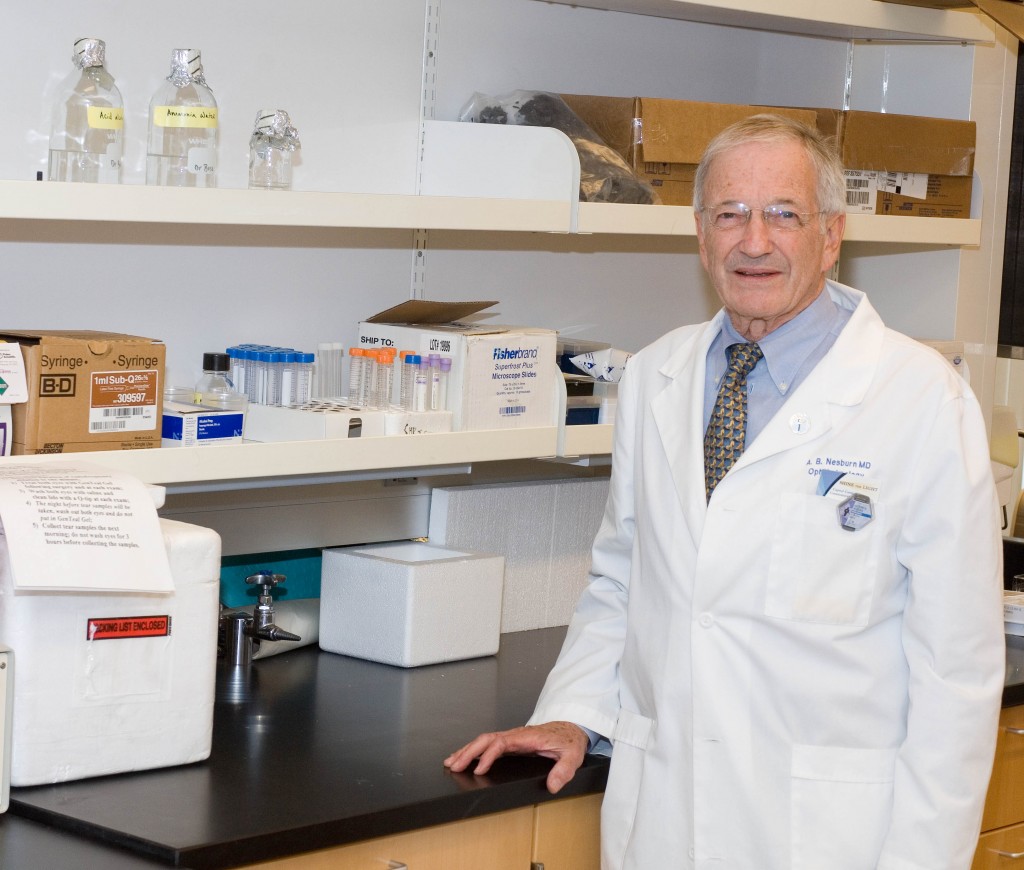
“I was brainwashed from the age of 5,” says Dr. Anthony Nesburn, medical director of The Discovery Eye Foundation (DEF). “My dad would take me on rounds at the hospital and to his office. He introduced me to medicine at a really early age.”
Nesburn received a telegram while he was an undergrad at UCLA, telling him he’d been accepted to Harvard Medical School. His mother started crying: “You’re going to Boston! We’re not going to see you anymore!” While he “was loathe to leave Southern California,” Harvard was too good to pass up.
Drafted by the Army out of his ophthalmology residency at Harvard in 1960, Nesburn joined the Navy instead. He followed in his father’s footsteps again, becoming a Navy flight surgeon. (Henry had volunteered during World War II.)
He went on to a Boston Children’s Hospital fellowship in infectious disease, working with Nobel laureate Dr. John Enders, whose work led to the polio vaccine and changed the face of virology. Nesburn then did his residency at Massachusetts Eye and Ear. “I was part of a special program that allowed us to do research, and I was running a research laboratory while I was a resident,” he says. “It gave me the start I needed.”
“At Mass Eye and Ear, I worked for an up-and-coming ophthalmologist and researcher to prove there was a substance that could treat herpes eye infections. We wrote a paper that included the very first antiviral ever described, and it was against herpes virus. It is the basis for today’s herpes antivirals,” Nesburn says. “I was hooked.”
He went back to Los Angeles and received NIH funding to continue his research on ocular herpes. In 1968, he joined his father’s practice half-time, spending the rest of his time doing research.
Two years later, he received a generous offer, when Rita and Morris Pynoos started DEF to fund his research. The Pynooses were grateful to Nesburn for diagnosing their son, Jon, with keratoconus (KC). “I was a second-year resident at Mass Eye and Ear, and Jon Pynoos was an undergraduate at Harvard. His parents went to see my dad, because Jon couldn’t see well, and no one could figure out what was wrong with his vision. My dad said, ‘Send him over to Tony; he’ll figure out what’s going on!’ I said to myself, ‘Holy mackerel! What happens if he has something really complicated? I’m just a newbie!’” Nesburn remembers. “Jon came in; I looked at him, and the keratoconus was so clear and easy to spot. I couldn’t imagine how his doctors didn’t see it. We got him contact lenses, and he was able to see again. When I came back to LA, the Pynooses wanted to do something to help.”
At first, DEF research focused on KC and the herpes research Nesburn was working on at the time. It soon broadened to include macular degeneration and retinal disease.
“My dad had to retire from the practice of ophthalmology at the age of 70, because of bad age-related macular degeneration (AMD). His mother and older sister had had it, as did several cousins. There was no treatment back then that helped,” Nesburn says.
“AMD is the most common cause of permanent vision loss in the elderly in the developed world. I could see where the need was,” he says. “We moved forward at DEF with two driving mantras: We wanted to do something significant in macular degeneration research and to find the cause of keratoconus.”
As a virologist in research and a corneal surgeon, Nesburn realized he needed a corneal biochemist to help with the KC research. He met Dr. Cristina Kenney at an Association for Research in Vision and Ophthalmology meeting. She joined DEF, and within 15 years, they found the chemical cause of keratoconus; they also got married.
Now nearly 80 years old, Nesburn spends most of his time “wearing three hats”: fundraising for DEF, lab research and clinical practice. His daughter, Kristin, is the third generation to join the family ophthalmology practice.
“While I’m still able, I want to try to make a difference in medicine, particularly in macular degeneration,” Nesburn says. “Macular degeneration affects so many people. This is where I want to put my energy. Luckily, as strong as it is in our family, I don’t have it … yet.
“As a researcher, my interest in putting together a program for macular-degeneration diagnosis and treatment has been because it’s a great public health problem. Yes, if I should ever get it, it might be able to help me or my family, but the first thing, as a scientist, is to try to get something to help humankind. I know it sounds sappy, but it’s true.”
3/26/15
 Anthony B. Nesburn, MD, FACS
Anthony B. Nesburn, MD, FACS
Medical Director, Discovery Eye Foundation
Professor & Vice Chairman for Research, Ophthalmology
Gavin Herbert Eye Institute, University of CA, Irvine