There is an old Irish ditty I often heard as a little boy. It goes something like this:
“One bright and guiding light that taught me wrong from right I found in my mother’s eyes. Those baby tales she told of roads all paved with gold I found in my mother’s eyes”.
As a blind child there was so much I found in my mother’s eyes. From as early as I can remember, she read me stories that spanned from Robert Lewis Stephenson’s adventures like “Treasure Island” to the book that always made both of us cry – “Black Beauty.”
As a teenager and young adult, her eyes made it possible for me to venture into the world knowing as she liked to say…”dressed to the nines.” And then, when I married my wife, Patty, my mother had strong opinions about the choice of tuxedo I should wear on our wedding day. I can still remember hearing her talk about how much she loved to see the first smiles on the faces of our children, Blythe & Tom.
As she grew older, it was her eyes that kept her connected to the world. Every morning, she read her Boston Globe from cover to cover, and on afternoon television she never missed her Soap Operas – “The Guiding Light,” and “Search for Tomorrow.” And then, there was the NBC Nightly News with her on-going crush on Tom Brokaw.
April is Women’s Eye Health Month along with celebrating the need for Sports Eye Safety. I can still remember my mother crying when she watched Cleveland Indian’s left-handed pitcher Herb Score hit with a line-drive costing him his sight. Research goes hand in hand with eye-safety to preserve vision. The Discovery Eye Foundation is committed to finding the answers that will preserve vision and allow women and mothers the blessing of seeing the smiles on the faces of the children they love.


 Tom Sullivan
Tom Sullivan

 The other day my daughter Blythe asked me which Christmas I consider to be my favorite. I had to think a minute, because as a family, the Sullivan’s have had some great ones. I was about to say the first time you and your brother Tom were old enough to really get into Santa, being absolutely sure that the fat man brought your presents right down the chimney. I was about to say that, and then I remembered.
The other day my daughter Blythe asked me which Christmas I consider to be my favorite. I had to think a minute, because as a family, the Sullivan’s have had some great ones. I was about to say the first time you and your brother Tom were old enough to really get into Santa, being absolutely sure that the fat man brought your presents right down the chimney. I was about to say that, and then I remembered.  Colorado, when our children were teenagers and our friend, the marvelous Betty White, joined us for a Christmas Eve sleigh ride none of us will ever forget. The night was perfect. It had snowed earlier that day, and the air had a feeling of Christmas that you could almost taste. Oh, sure, it was cold, but we were bundled up under tons of blankets as two beautiful Clydesdale horses with bells jingling took us through the woods to a magical barn where dinner would be served and carols sung.
Colorado, when our children were teenagers and our friend, the marvelous Betty White, joined us for a Christmas Eve sleigh ride none of us will ever forget. The night was perfect. It had snowed earlier that day, and the air had a feeling of Christmas that you could almost taste. Oh, sure, it was cold, but we were bundled up under tons of blankets as two beautiful Clydesdale horses with bells jingling took us through the woods to a magical barn where dinner would be served and carols sung.  Harsh weather conditions can reduce the natural moisture in your eyes and the irritation usually results in a burning or itching sensation that often leads to rubbing or scratching your eyes which can worsen the symptoms. Sometimes it feels like there is a foreign object in your eye and for some, dry eyes can even cause excessive tearing, as your eyes try to overcompensate for their lack of protective tears. Prolonged, untreated dry eyes can lead to blurred vision as well. Between the harsh winter winds outside and the dry heat radiating inside, our eyes are very quickly irritated and dried in the winter months. The result is itchy, dry eyes that may cause pain, blurred vision, a burning sensation, or even watery vision as our eyes try to compensate for the dryness.
Harsh weather conditions can reduce the natural moisture in your eyes and the irritation usually results in a burning or itching sensation that often leads to rubbing or scratching your eyes which can worsen the symptoms. Sometimes it feels like there is a foreign object in your eye and for some, dry eyes can even cause excessive tearing, as your eyes try to overcompensate for their lack of protective tears. Prolonged, untreated dry eyes can lead to blurred vision as well. Between the harsh winter winds outside and the dry heat radiating inside, our eyes are very quickly irritated and dried in the winter months. The result is itchy, dry eyes that may cause pain, blurred vision, a burning sensation, or even watery vision as our eyes try to compensate for the dryness. I can only imagine my wife’s beautiful face. Oh sure, I’ve touched it and kissed it many times. I’ve felt the lines with the tips of my fingers, tracing our lives together, and I’ve heard her smile. I understand that’s not really seeing it. It’s not seeing her eyes as they sparkle with something funny I said; or, when she looks at me with love reserved only for those who are truly in love.
I can only imagine my wife’s beautiful face. Oh sure, I’ve touched it and kissed it many times. I’ve felt the lines with the tips of my fingers, tracing our lives together, and I’ve heard her smile. I understand that’s not really seeing it. It’s not seeing her eyes as they sparkle with something funny I said; or, when she looks at me with love reserved only for those who are truly in love.
 Costume Contact Lenses such as cat eyes or zombie may make your Halloween costume a bit more frightful although wearing those lenses without a prescription can be more terrifying, as it could result in vision loss or even blindness.
Costume Contact Lenses such as cat eyes or zombie may make your Halloween costume a bit more frightful although wearing those lenses without a prescription can be more terrifying, as it could result in vision loss or even blindness.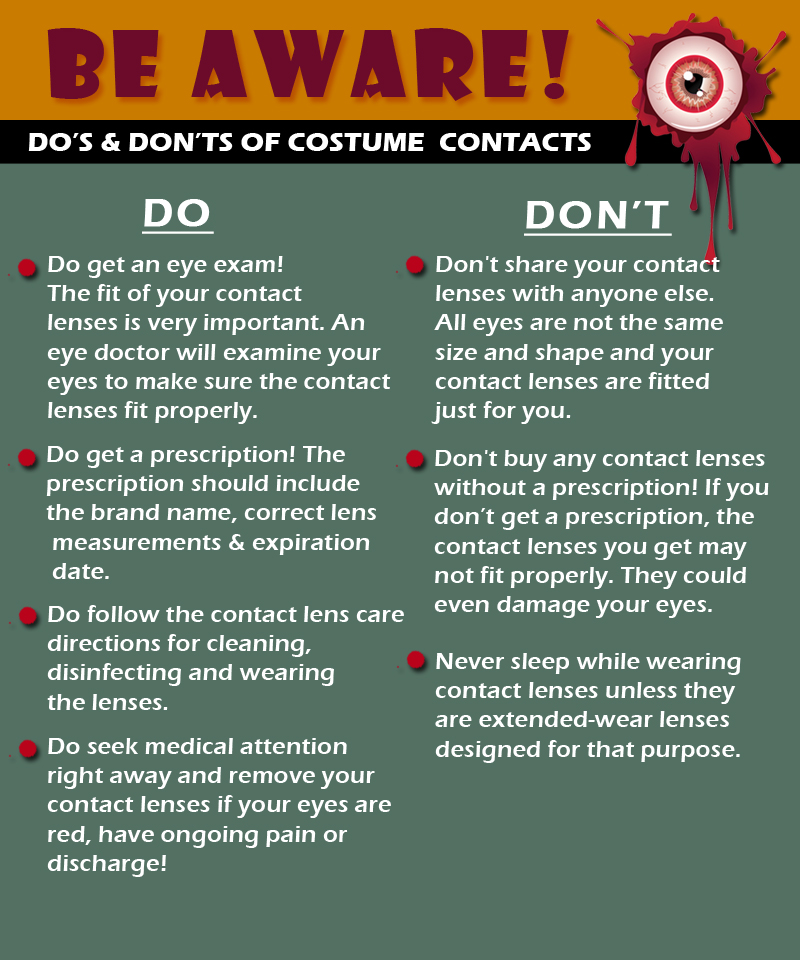

 Tom Sullivan
Tom Sullivan
 The Difference Between an
The Difference Between an