This has been a cold winter so far, and since it is only January, it is bound to get colder. The extreme cold, combined with winds, snow, rain and other environmental factors, can really take a toll on your eyes. And while it may be snowing or raining, winter air is actually drier than any other season. This can be especially difficult if you wear contact lenses. Here is what you should know about wearing contact lenses in winter.
This has been a cold winter so far, and since it is only January, it is bound to get colder. The extreme cold, combined with winds, snow, rain and other environmental factors, can really take a toll on your eyes. And while it may be snowing or raining, winter air is actually drier than any other season. This can be especially difficult if you wear contact lenses. Here is what you should know about wearing contact lenses in winter.
- Wear sunglasses for protection from UV rays and wind. Your eyes can become sunburned which cause blurry vision and can make your eyes feel like they are burning (think of your sunburned skin feels) for 24 to 72 hours. It will also protect your eyes from snow, rain or anything else the wind can send your way.
- Avoid direct sources of heat such as heating vents and fireplaces. Indoor heating can draw the moisture out of the air, so consider a humidifier to help maintain the correct amount of moisture in the air to help keep eyes moist. Cool-air humidifiers have less of a tendency toward mold and bacteria.
- Speaking of hydration, we also tend to drink less water in the winter months, so make a concentrated effort to keep up your water intake.
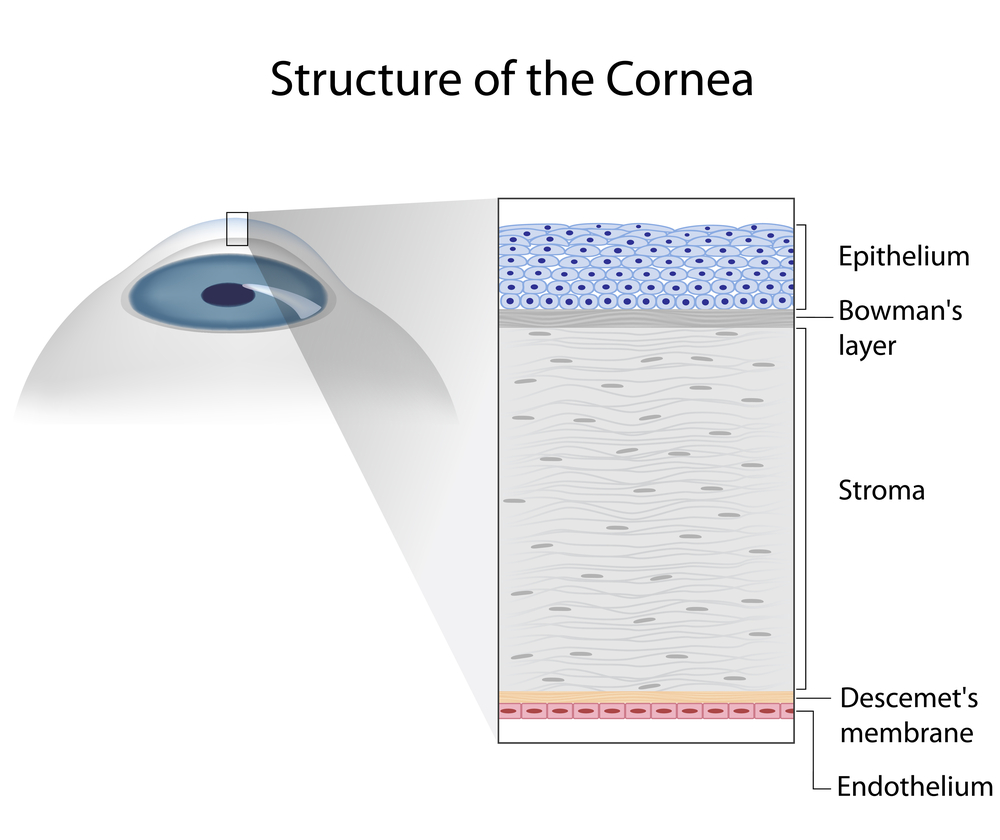
- If it is so dry, why are my eyes watering? This is a common question and the answer may be a bit counter-intuitive. Anything that irritates your eyes, including dryness, causes a tearing reflex. Your tear glands go into overdrive trying to replace the moisture to your cornea. To try and reduce the tearing, you can use eye drops or artificial tears specifically designed for use with contact lenses.
- Your eyes are not the only thing that dries out in the winter, so does your skin. Try to put in your contacts before moisturizing your skin, especially your hands. So wash your hands, put in your lenses and then use your creams and lotions.
- Change out your contact lenses regularly in cold weather according to the recommended schedule, be it daily, every two weeks or monthly. This will allow them to better conduct oxygen, reduce irritation and increase comfort.
- Take a break from your contacts and wear your eyeglasses. Putting them on when you get home from work can make a big difference. Contact lenses dry your eyes out on their own, when you add cold weather it gets that much worse.
- Get plenty of sleep, which also helps with the dryness and fatigue. This will help you start the day with your eye refreshed and ready for the many things you will put them through throughout the day ahead.
Do you have any other suggestions that have helped you cope when wearing contact lenses in winter?
1/15/16
 Susan DeRemer, CFRE Vice President of Development Discovery Eye Foundation
Susan DeRemer, CFRE Vice President of Development Discovery Eye Foundation