Healthy Aging Month is an annual health observance designed to focus national attention on the positive aspects of growing older. Aging is a process that brings many changes. Vision loss and blindness, however, do not have to be one of them. There are several simple steps you can take to help keep your eyes healthy for the rest of your life.
Healthy Aging Month is an annual health observance designed to focus national attention on the positive aspects of growing older. Aging is a process that brings many changes. Vision loss and blindness, however, do not have to be one of them. There are several simple steps you can take to help keep your eyes healthy for the rest of your life.
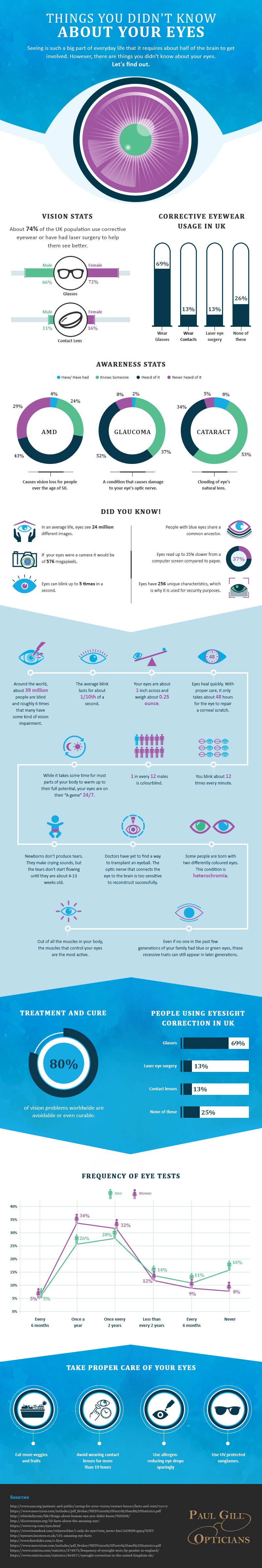
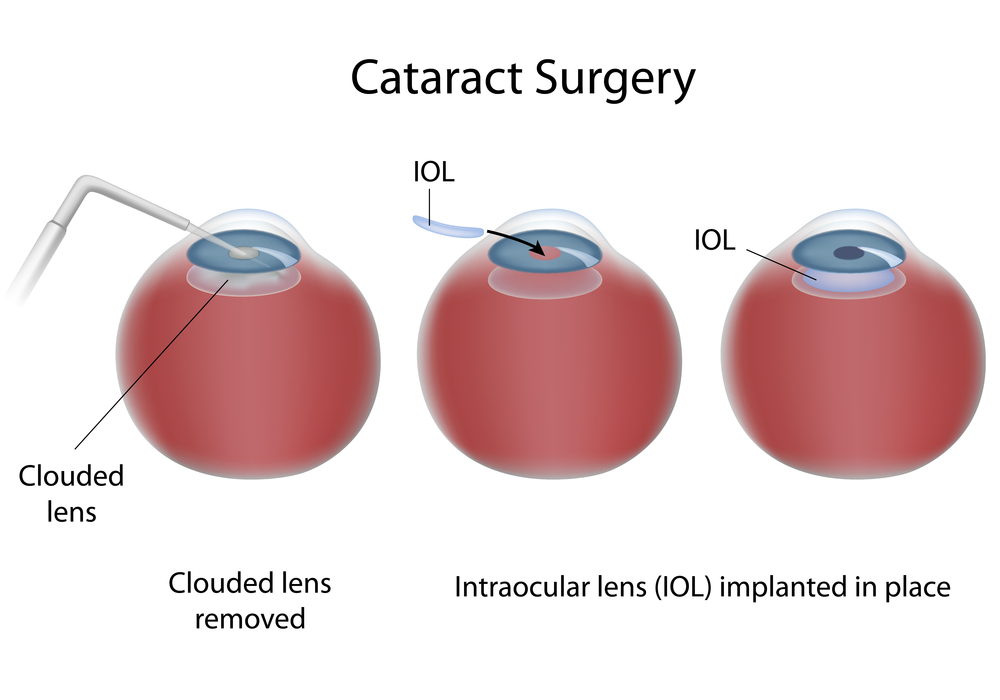
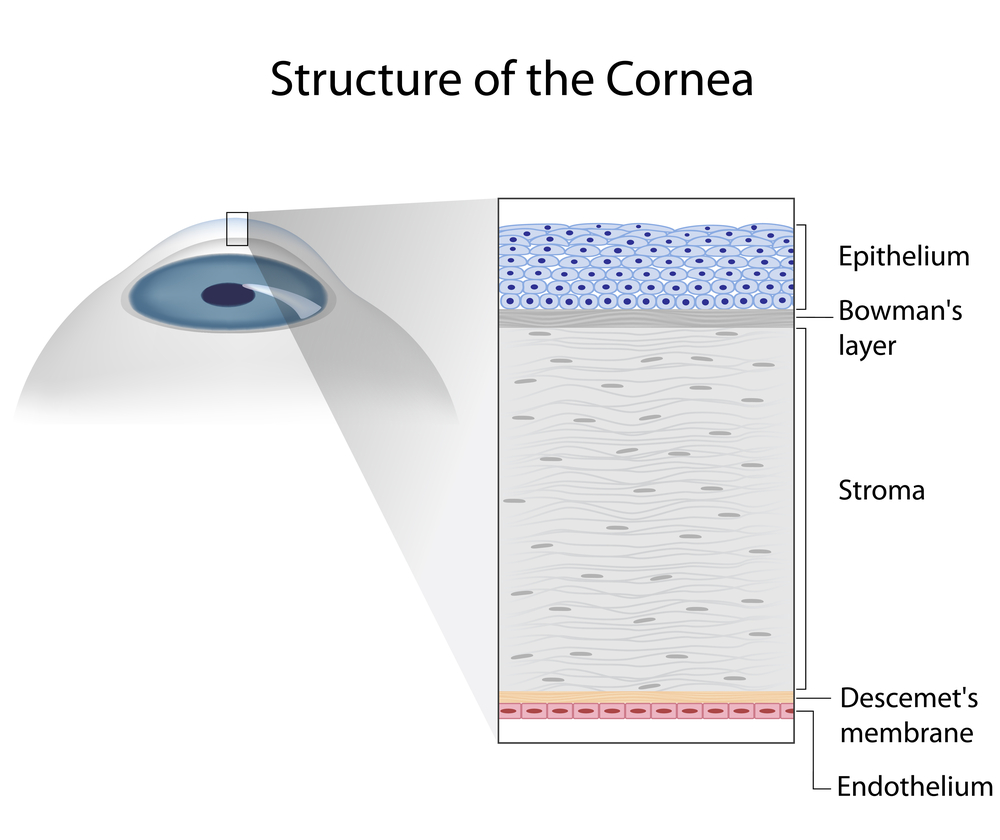
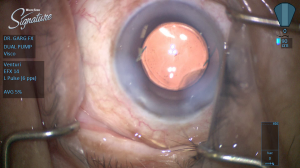
Eye diseases often have no early symptoms, but can be detected during a comprehensive dilated eye exam. A comprehensive dilated eye exam is different from the basic eye exam or screening you have for glasses or contacts. By dilating the pupils and examining the back of the eyes, your eye care professional can detect eye diseases in their early stages, before vision loss occurs. By performing a comprehensive eye exam, your eye care professional can check for early signs of –
Here are some other tips to help maintain healthy vision and body now and as you age:
- Eat a healthy, balanced diet. Loading up on fruits and vegetables can help keep your eyes healthy and disease free.
- Maintain a healthy weight. Being overweight increases your risk for heart disease and diabetes. Complications from diabetes, such as diabetic retinopathy or glaucoma, can eventually lead to vision loss.
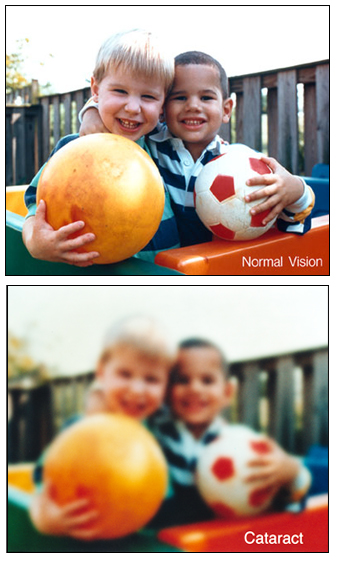
- Don’t smoke. Smoking increases your risk for age-related macular degeneration, cataract, and other systemic diseases, including cancer. Wear protective eyewear when outdoors. Protecting your eyes from the sun’s ultraviolet rays when you are outdoors is important for your eye health. Choose sunglasses that block 99 to 100 percent of both UV-A and UV-B radiation.
Even if you are not experiencing vision problems, visiting an eye care professional regularly for a comprehensive dilated eye exam is the most important thing you can do to reduce your risk of vision loss as you age.
Download “Everyone’s vision can change with age”
A handout with explanation on how vision can change with age.


 At the Discovery Eye Foundation (DEF), we are committed to supporting research that we believe will make the treatment of many forms of vision loss far more predictable and successful.
At the Discovery Eye Foundation (DEF), we are committed to supporting research that we believe will make the treatment of many forms of vision loss far more predictable and successful.  Tom Sullivan
Tom Sullivan