National Cataract Awareness Month is celebrated in June. The awareness campaign promotes information about the eye condition that is the leading cause of treatable vision loss in the U.S. Yes, this is a scary fact, but no need to be frightened because cataracts are treatable with an outpatient surgery, which has over a 97% success rate.*
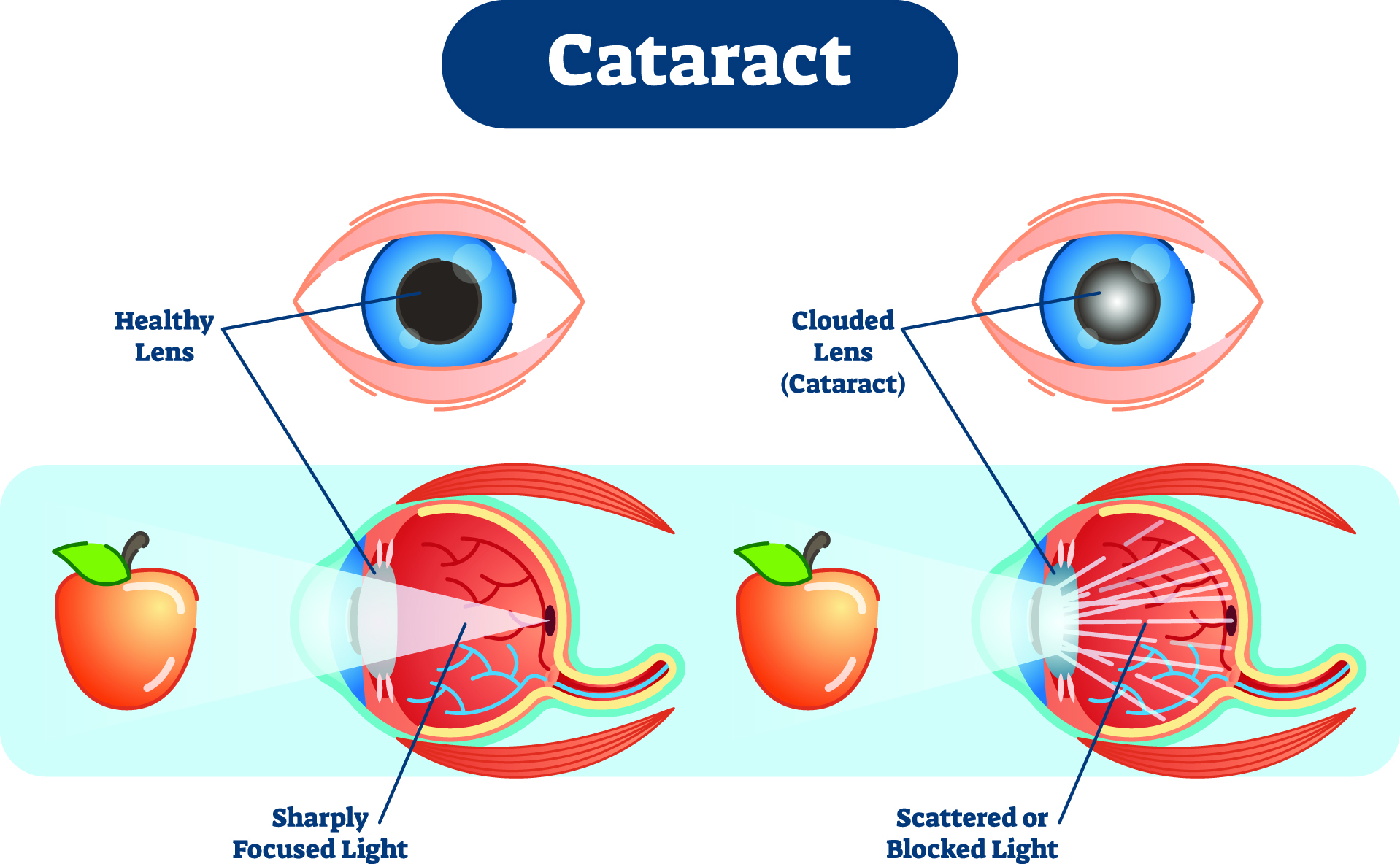
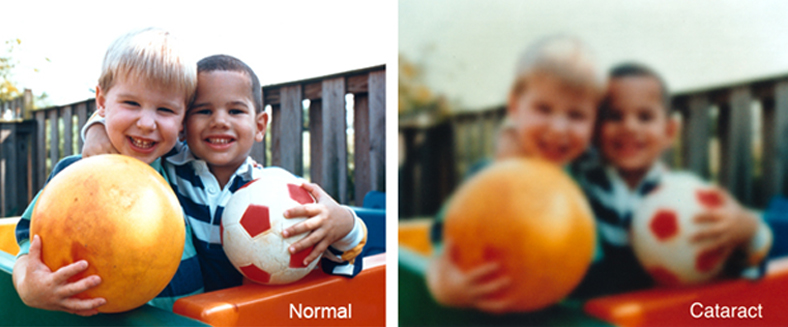
Vision loss from cataract is caused by clouding on the lens of the eye. Cataract surgery removes the cloudy lens and replaces it with a crystal-clear artificial lens. This common eye condition mostly affects people over 50 and the causes can range from simple aging, diabetes, long-term eye diseases, and eye injury/inflammation, to factors like hereditary influences, smoking, intake of certain oral steroids, and so forth.
Although there may be no early symptoms, patients may begin to notice:
- cloudy or blurry vision
- colors that look faded
- difficulty seeing at night
- a halo around lights, making night driving difficult
- seeing double out of the affected eye
- frequent changes of the prescription of eyeglasses or contact lenses
YOUR DIET IS VERY IMPORTANT
A healthy diet may help reduce risk of and/or delay formation and progression of cataracts. Research suggests that a diet high in vitamin C-rich foods — citrus (oranges, kiwi, lemon, grapefruit), bell peppers, strawberries, tomatoes, cruciferous vegetables (broccoli, Brussels sprouts, cabbage, cauliflower) — is helpful in slowing the progression of cataracts. More importantly, adopting good nutrition is a cornerstone of optimizing health early in life and can greatly reduce the risk of developing age-related diseases including cataracts. For eye healthy recipes visit discoveryeye.org/eye-cook-delicious-food-health/
BE SURE TO HAVE AN ANNUAL EYE EXAM
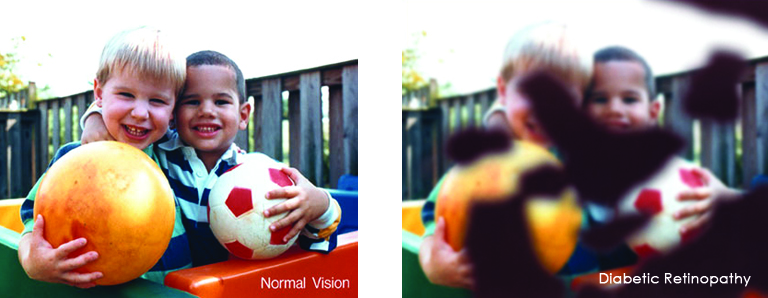
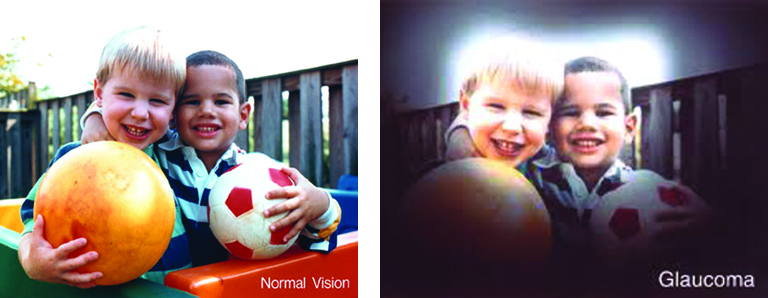
By age 40, all adults should visit an eye specialist for a comprehensive eye exam to screen for early-stage cataracts and other eye diseases that are leading causes of low vision and even blindness. By age 65, a routine eye exam is recommended every year, in most cases to diagnose cataracts that are progressively clouding the lens. A comprehensive eye exam allows eye specialists to detect and monitor cataract progression as well as diagnosing other problems such as glaucoma. Patients should discuss with their eye specialist their vision problems and seek guidance about the timing of cataract surgery when worsening vision has compromised their quality of life and normal functioning.
LIVE A HEALTHY LIFESTYLE
Multiple factors are at play that increase our risk for developing a degenerative eye disease or vision compromising conditions as we age. If an individual lives long enough, then cataract formation is unavoidable. Living a healthy lifestyle, however, greatly improves an adult’s odds of avoiding early onset, faster progression, or possibly even avoiding the need for cataract surgery in the future.
WHY WE PROMOTE CATARACT AWARENESS MONTH
- It’s a celebration of sight – The ability to see the world clearly and in all its glory is something we shouldn’t take for granted. Millions upon millions of cells perform complex operations in our eyes to allow us the gift of sight. We should take care of our eyes and appreciate our glorious vision for what it is.
- It’s a celebration of science – Science has not only explained to us how intricately our eyes work, but it has also revealed to us the many ways we can repair and treat them in case things go south. Medical advancements have ensured that about 80% of all eye diseases are treatable or can be prevented.
- It’s a celebration of modern surgery – There’s “always” light at the end of the tunnel. Today’s cataract surgery is a modern day miracle developed by dedicated surgeons over the last five decades. For most of us it is a painless, outpatient surgery with rapid return of excellent vision.
* https://my.clevelandclinic.org/health/treatments/21472-cataract-surgery
For more information about cataract:
https://discoveryeye.org/eye-conditions/cataracts/



 Harsh weather conditions can reduce the natural moisture in your eyes and the irritation usually results in a burning or itching sensation that often leads to rubbing or scratching your eyes which can worsen the symptoms. Sometimes it feels like there is a foreign object in your eye and for some, dry eyes can even cause excessive tearing, as your eyes try to overcompensate for their lack of protective tears. Prolonged, untreated dry eyes can lead to blurred vision as well. Between the harsh winter winds outside and the dry heat radiating inside, our eyes are very quickly irritated and dried in the winter months. The result is itchy, dry eyes that may cause pain, blurred vision, a burning sensation, or even watery vision as our eyes try to compensate for the dryness.
Harsh weather conditions can reduce the natural moisture in your eyes and the irritation usually results in a burning or itching sensation that often leads to rubbing or scratching your eyes which can worsen the symptoms. Sometimes it feels like there is a foreign object in your eye and for some, dry eyes can even cause excessive tearing, as your eyes try to overcompensate for their lack of protective tears. Prolonged, untreated dry eyes can lead to blurred vision as well. Between the harsh winter winds outside and the dry heat radiating inside, our eyes are very quickly irritated and dried in the winter months. The result is itchy, dry eyes that may cause pain, blurred vision, a burning sensation, or even watery vision as our eyes try to compensate for the dryness.
 FIREWORK & EYE SAFETY:
FIREWORK & EYE SAFETY:  Even sparklers can be dangerous, as they burn at more than 2,000 degrees Fahrenheit. Sparklers were responsible for 900
Even sparklers can be dangerous, as they burn at more than 2,000 degrees Fahrenheit. Sparklers were responsible for 900  As winter shifts to spring, and flowers, grasses and trees begin to bloom, spring can take a toll on your eyes if you suffer from seasonal allergies. The spring season has a marked an increase in pollen and allergens in the air, that leave you with congestion, headaches, and itchy, swollen eyes, known as eye allergies.
As winter shifts to spring, and flowers, grasses and trees begin to bloom, spring can take a toll on your eyes if you suffer from seasonal allergies. The spring season has a marked an increase in pollen and allergens in the air, that leave you with congestion, headaches, and itchy, swollen eyes, known as eye allergies.