 Your eyes are delicate and constantly at work, yet many everyday habits can unknowingly contribute to long-term damage to our vision. Here are 10 everyday habits that might be harming your eyes without you even realizing it:
Your eyes are delicate and constantly at work, yet many everyday habits can unknowingly contribute to long-term damage to our vision. Here are 10 everyday habits that might be harming your eyes without you even realizing it:
- Rubbing your eyes – This can damage the delicate tissues around the eyes and increase the risk of keratoconus in susceptible people. It also spreads germs, raising the chance of infections like conjunctivitis.
Better habit: Use a clean tissue or wash your face if your eyes are irritated.
- Staring at screens for too long – Spending hours on phones, computers, or tablets without breaks can cause digital eye strain. Symptoms include dryness, blurred vision, headaches, and eye fatigue.
Better habit: Follow the 20-20-20 rule — every 20 minutes, look at something 20 feet away for 20 seconds.
- Sleeping in contact lenses – Wearing contacts overnight (unless specifically approved) can cut off oxygen to your corneas and increase the risk of corneal ulcer.
Better habit: Always remove and clean contacts before bed.
- Skipping sunglasses – Not wearing sunglasses exposes your eyes to harmful UV rays, increasing the risk of cataract and macular degeneration over time.
Better habit: Wear sunglasses that block 100% of UVA and UVB rays, even on cloudy days.
- Ignoring dryness or irritation – Eye dryness can lead to chronic discomfort or damage to the corneal surface if left untreated. It may be linked to dry eye syndrome.
Better habit: Use preservative-free artificial tears and blink more often, especially when using screens. If persists, see your eye care practitioner.
- Not removing makeup properly – Sleeping in eye makeup can block oil glands, causing irritation or infection.
Better habit: Gently remove makeup each night with a clean cloth or wipes designed for the eye area.
- Using expired eye makeup – Old makeup can harbor bacteria, leading to eye infections.
Better habit: Replace mascara every 3 months and avoid sharing makeup to reduce the risk of contamination.
- Poor Contact Lens Hygiene – Not cleaning your contact lenses properly or using tap water to rinse them can lead to infections.
Better habit: Always follow your eye doctor’s care instructions, use fresh solution, and wash your hands before handling lenses.
- Reading in Poor Lighting – Though it won’t permanently damage your eyes, reading in dim light can cause eye strain and discomfort.
Better habit: Read or do close up work with adequate lighting.
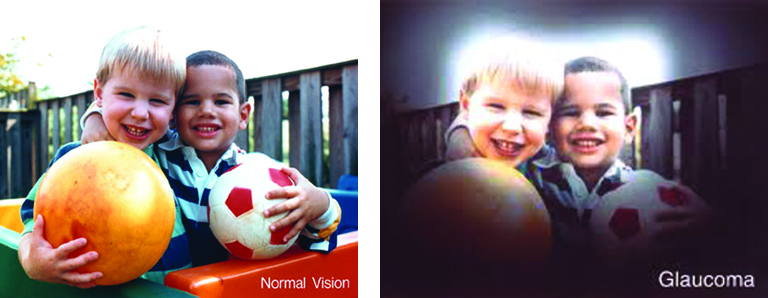
- Skipping regular eye exams – Some serious eye diseases, like glaucoma, can develop without noticeable symptoms.
Better habit: Get a comprehensive eye exam every 1–2 years (or as recommended by your eye doctor).
Taking care of your eyes is just as important as caring for the rest of your body. Breaking bad habits and staying on top of regular eye exams can help keep your vision strong for years. If you have any concerns about your eye health, consult your eye care professional for advice.


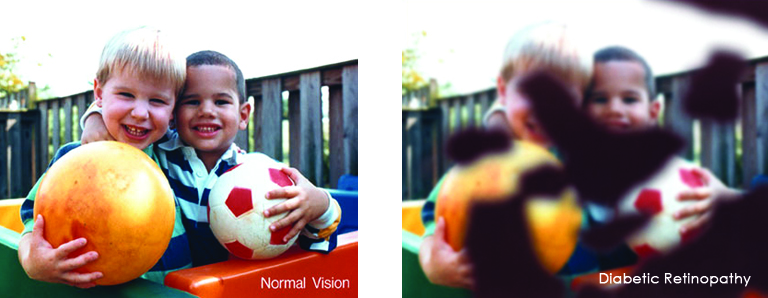
 Low vision affects millions of Americans — including many older adults. People with low vision aren’t blind, but because of their vision loss, they may not be able to do everyday tasks like driving or reading even with glasses.
Low vision affects millions of Americans — including many older adults. People with low vision aren’t blind, but because of their vision loss, they may not be able to do everyday tasks like driving or reading even with glasses.

 Tom Sullivan
Tom Sullivan



 When you think of cancer, most of us do not think about the eye or vision. Though rare, cancer can start inside or outside of the eye. If cancer starts inside the eyeball it’s called intraocular and if it starts outside the eye (eyelid or in the eye socket) then it’s called extraocular tumor. It can occur in both children and adults. Most major eye centers have specialists who are trained in the diagnosis and treatment of eye cancers.
When you think of cancer, most of us do not think about the eye or vision. Though rare, cancer can start inside or outside of the eye. If cancer starts inside the eyeball it’s called intraocular and if it starts outside the eye (eyelid or in the eye socket) then it’s called extraocular tumor. It can occur in both children and adults. Most major eye centers have specialists who are trained in the diagnosis and treatment of eye cancers.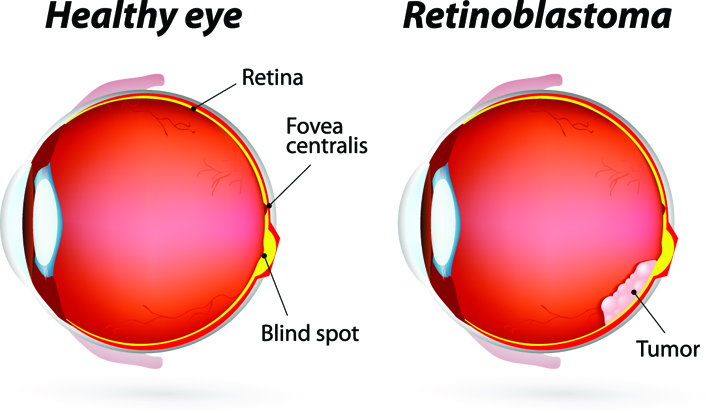 At the later stage of this cancer, the only one way to survive is to remove the eyeball (enucleation). Like many of other types of cancer, retinoblastoma has a genetic component so genetic testing needs to be done. The tumor begins with the RB1 gene mutation that stimulates retinal cells to develop into a tumor called a retinoblastoma. The RB1 mutation can be inherited from the parents, but in some cases it is sporadic and not inherited. There are various treatments such as surgery, chemotherapy, radiotherapy etc. to cure retinoblastoma cancer. Rarely it can spread beyond the eye.
At the later stage of this cancer, the only one way to survive is to remove the eyeball (enucleation). Like many of other types of cancer, retinoblastoma has a genetic component so genetic testing needs to be done. The tumor begins with the RB1 gene mutation that stimulates retinal cells to develop into a tumor called a retinoblastoma. The RB1 mutation can be inherited from the parents, but in some cases it is sporadic and not inherited. There are various treatments such as surgery, chemotherapy, radiotherapy etc. to cure retinoblastoma cancer. Rarely it can spread beyond the eye. 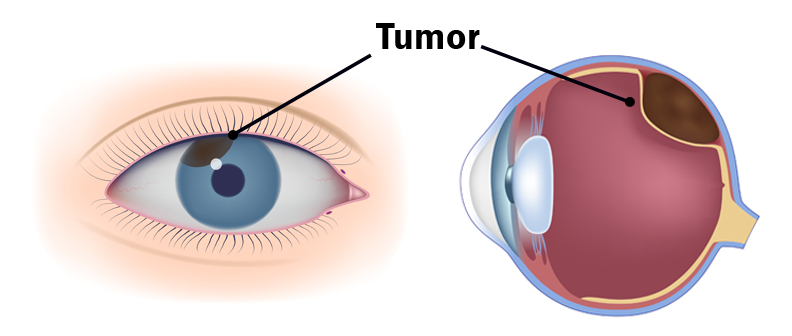
 Lauren Hauptman
Lauren Hauptman