10/23/14
The Discovery Eye Foundation Fall 2014 e-newsletter focused on depression and eye disease. At the time we asked for people that were willing to share their stories. Jennifer Villeneuve is one of the many that responded. She is 26 years old and lives in Ontario, Canada. A participant in KC-Link, she talks about the emotional toll keratoconus has taken on her life and living with KC.

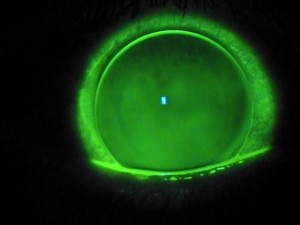
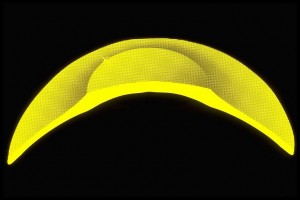
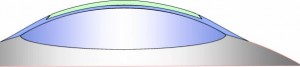
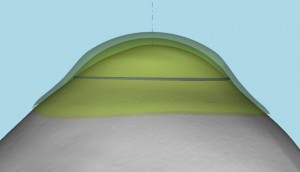
At age 13, I was diagnosed with keratoconus and given RGP lenses, with which I struggled intensely. ?I became very quiet, and my bubbly personality disappeared. The lenses often got irritated and made my eyes water and turn red, which made me look like I was crying. My doctor didn’t really give me much information on the disease. He just told me my corneas were the shape of footballs instead of circles.
I couldn’t be a normal teenager. I often squinted and had red eyes, which made me very self-conscious. I couldn’t wear makeup or have a free-for-all teenage life. I had to worry about my lenses and what people saw when they looked at me. Some people knew about my KC, but not many. I was just that quiet person who squinted. Because of this, my self-esteem got very low. All in all, my high-school life was hell.
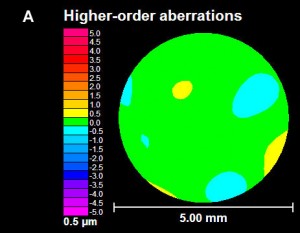
Every time I went to the doctor, he said my pain is normal, the discomfort is typical, and I needed to get used to it. I was also diagnosed with two learning disabilities, in addition to my vision impairment. Throughout high school, I had major anxiety and depression, though I never wanted to admit it. A close teacher even spoke to my mom about the anxiety and low self-esteem. I got through high school, still with the depression being untreated — and still with the same doctor who never even sent me for a topography scan. Each time I went in, it was, “Yup your eyes the same; see ya.”
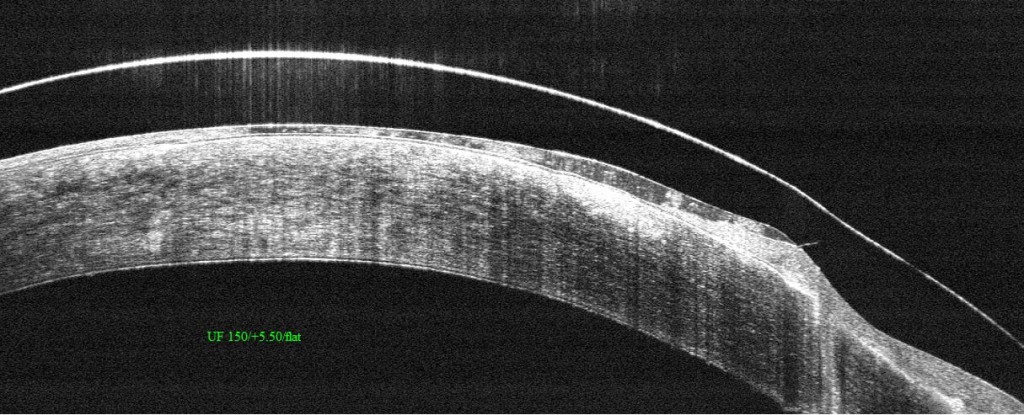
In college, I was diagnosed with depression and anxiety and was finally getting treated. ?I also went to the University of Ottawa Eye Institute of The Ottawa Hospital in Ontario, Canada. They did topographic scans; my KC had gotten significantly worse. My contacts’ sizing changed twice that year. Again, I couldn’t be normal. College students go out partying, but not me. I stayed in my room by myself. I worried whether I could see enough to go out. What if I drank too much and lost a lens? It wasn’t worth the risk, especially given how expensive they are. In college, I got great help and acceptance. My teachers all knew about my KC, and I was set up with the Centre for Students with Disabilities at Algonquin College in Ottawa. They were my backbone and my support.

After my two years in college, I moved on to my career working with children. At each job, I had to explain why I always had a mirror and my contact stuff. At first, I was ashamed and almost embarrassed, explaining why I squinted and that I may not be able to read a kids’ book if the writing is too small. Not only did I get accepted by coworkers, but also by the kids. They knew my eyes were red from my contacts or that my tears meant something was in my eye. I began working in with special-needs children, which was incredible but also challenging — especially in ensuring my eyes were at their best.
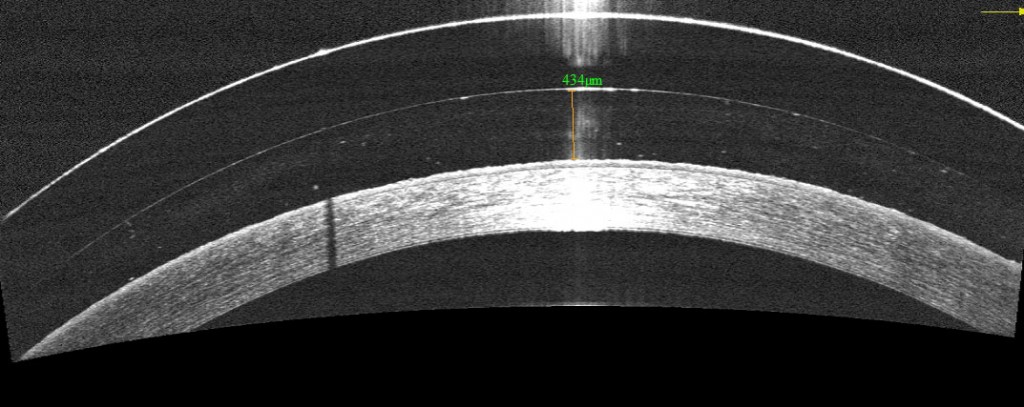
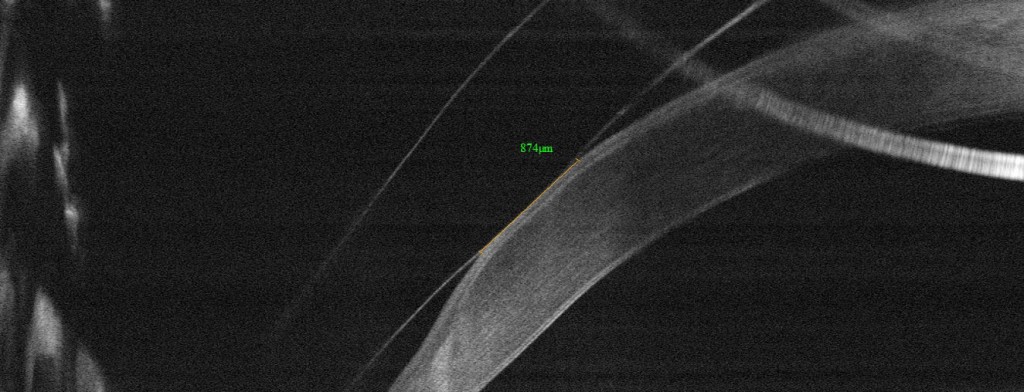
At this same time, my vision had gotten worse. I went for corneal crosslinking (CXL) in one eye. I had to take? time off from work, which caused a lot of stress. Unfortunately, there were complications from the CXL. I had a scar in the same eye that caused the crosslinking to be difficult and not as successful. When it came time to do my other eye, I was hesitant, but I needed it. It worked, and the disease slowed down.
A year or so later, the disease had a spike and caused my eye to rub on a lens and make a blister. I had laser surgery to get rid of that and the scar, too. Because KC isn’t covered by insurance in Ontario, I had to pay for every lens, every $11 bottle of solution and countless eye drops. It was expensive, and money was a struggle. I still struggle with the costs of things.
I also have to worry about eye infections. Since I work with kids, they are easy to get, but if I get an eye infection, I can’t wear my contacts, which means no driving, which means no working, which means no money. Things can snowball so quickly.
My vision is up and down. My lenses don’t last as long in my eyes as they used to, and my nighttime vision can be scary. I have to be extra-vigilant. Again, I can’t be normal or go somewhere unfamiliar at night. I’m always concerned. My lens fitter recently recommended scleral lenses, but I can’t afford them. I barely could afford the $2,000 for the CXL.
Living with KC isn’t easy. I can’t help but wonder how long I’ll have the vision I have now. Am I going to be blind in a few years? If I have children, will they have this, or will I even be able to see them? Will I find a guy who would want someone with the possibility of losing vision? I have to stop myself from thinking ahead, or the anxiety gets the best of me.