Being able to see clearly is important to all of us. But it is also something we have a tendency to take for granted until we notice changes in our vision. The point of the yearly comprehensive exam is to monitor your eyes before any problems arise, and address any concerns that could affect your vision later. Here is what to expect at your next comprehensive eye exam.
An eye exam involves an external examination of your eyes followed by a series of tests designed to evaluate your vision and check for eye diseases. Each test evaluates a different aspect of your vision and includes specific tests for visual acuity, pupil function, muscle function, visual fields, eye pressure and viewing the back of the eye through a dilated pupil.
External Exam
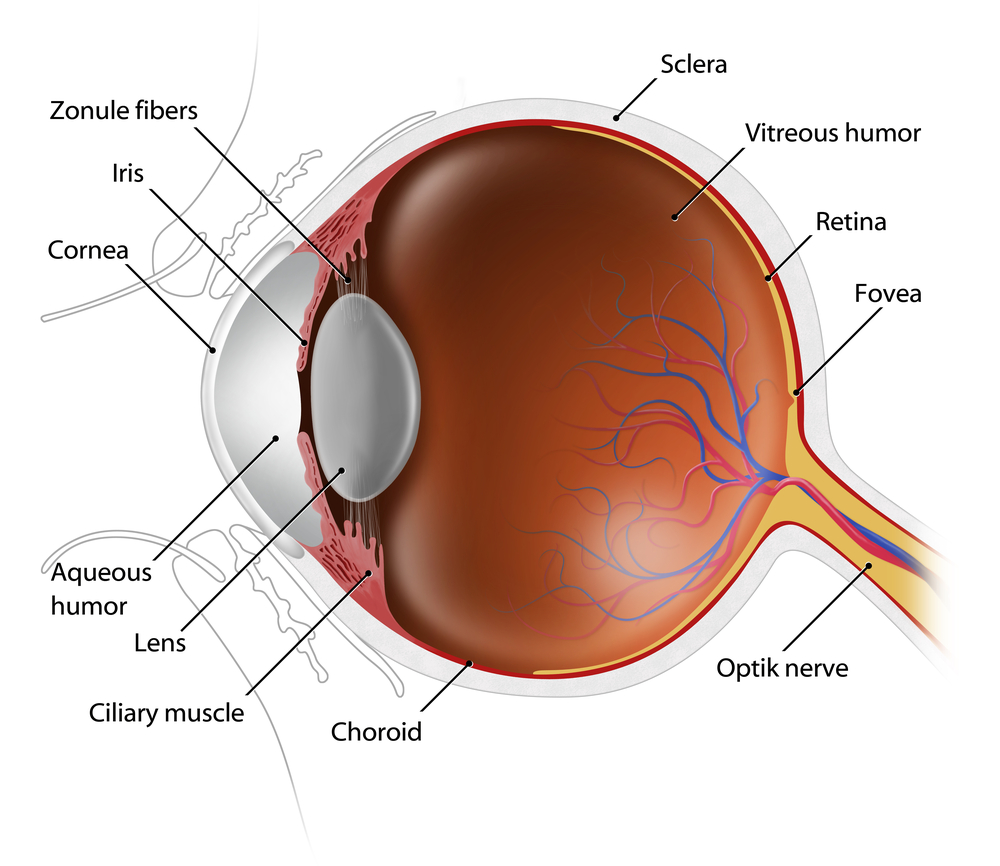
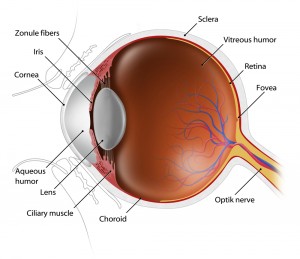
The external examination consists of inspecting the eyelids, surrounding tissues and the eyeball including the sclera (white part of the eye), iris and cornea.
Visual Acuity & Fields
Visual acuity is your eye’s ability to detect fine details and see an in-focus image at a certain distance. A Snellen chart and a phoropter are used. The standard definition of normal visual acuity is 20/20. The term 20/20 comes from even sized objects that can be seen by a “person of normal vision” at the specified distance. For example, if a person can see at a distance of 20 feet an object that normally can be seen at 20 feet, then they have 20/20 vision. If they can see at 20 feet what a normal person can see at 40 feet, then they have 20/40 vision. For the visual acuity test each eye is tested separately to gauge your side or peripheral vision.
the specified distance. For example, if a person can see at a distance of 20 feet an object that normally can be seen at 20 feet, then they have 20/20 vision. If they can see at 20 feet what a normal person can see at 40 feet, then they have 20/40 vision. For the visual acuity test each eye is tested separately to gauge your side or peripheral vision.
Pupil Function
An examination of the pupil begins with inspecting your pupils for equal size, regular shape, reaction to light, and direct and consensual reaction (meaning the pupil of one eye constricts when the other eye is exposed to light).
Eye Muscle Function
Eye movement is assessed two ways. First by having you move your eye quickly to a target at the far right, left, top and bottom. Then by slow tracking which uses the ‘follow my finger’ test, which tests all the muscles that move your eye.
 Eye Pressure Measurement
Eye Pressure Measurement
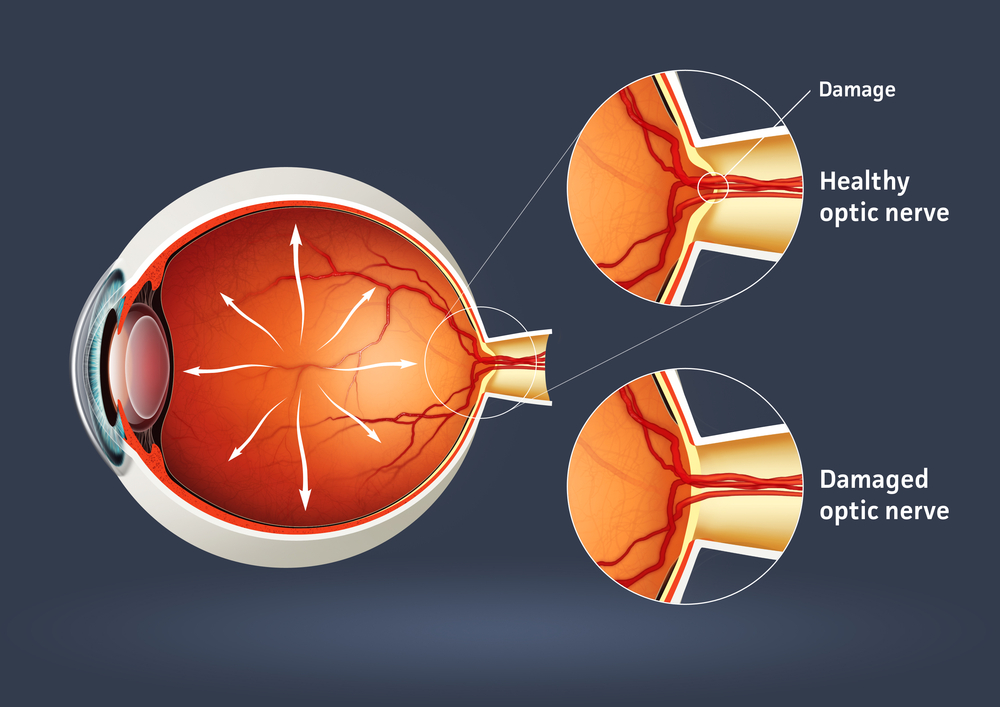
Intraocular pressure, or IOP, is measured using a tonometer to determine the fluid pressure inside your eye. This test provides information regarding your potential for glaucoma.
Viewing the Back of the Eye
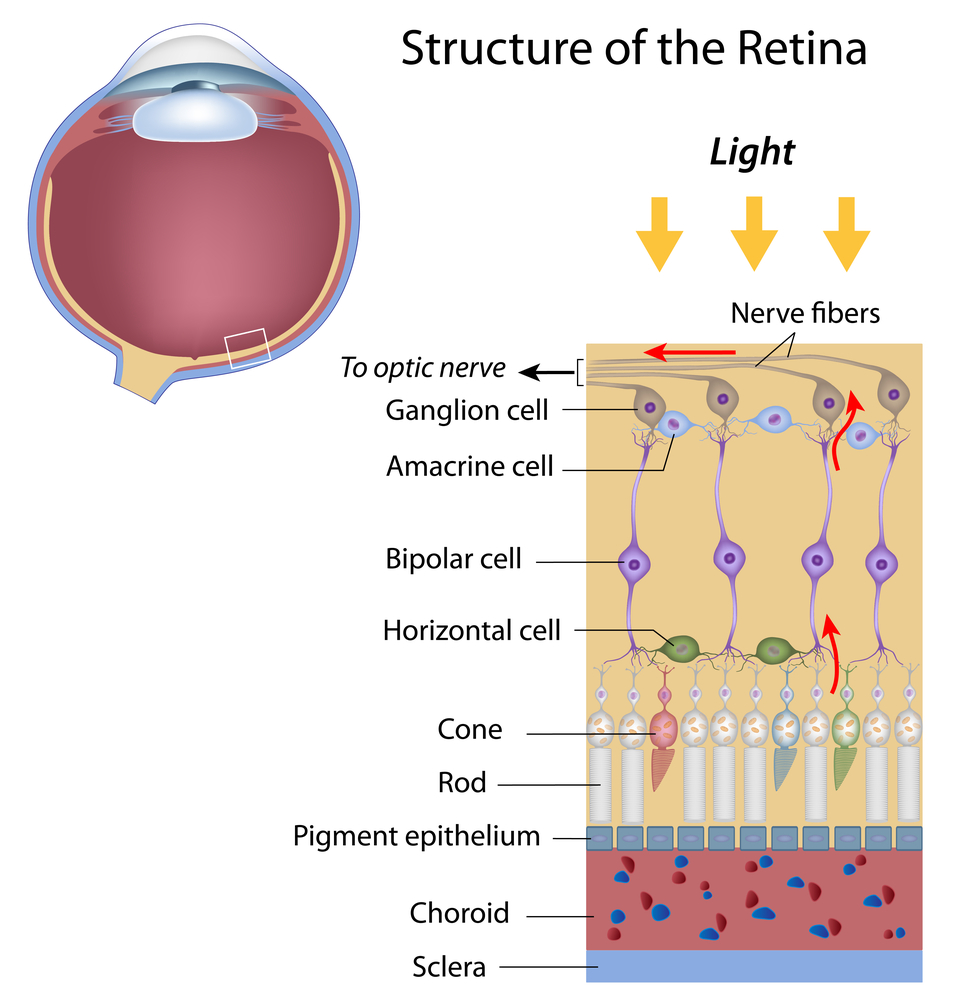
Increasing the size of your pupil with eye drops (known as dilating your eyes) allows the doctor to have a larger view of the back of your eye, including the retina, as demonstrated by this diagram. This is very important for diagnosis and tracking of macular degeneration and diabetic retinopathy.
Eye Structure
A special, high-powered microscope, called a slit-lamp, is used to view the structures of your eye clearly and in detail, enabling early diagnosis of a variety of eye conditions such as cataracts, presbyopia and corneal injury.
Taking care of your eyes, especially as you become older, is very important. Changes in vision may be gradual, or fast, but in both cases, early diagnosis is key to successful treatment and retaining your vision. It is suggested that individuals 40 and over have a comprehensive eye exam every one to two years. Exceptions would be if you have diabetes, in which case you should see your eye doctor yearly; or there is a family history of eye diseases such as glaucoma, macular degeneration, or corneal diseases, which may require more frequent visits to your eye doctor. If you have any degree of sudden vision loss, eye pain, or significant irritation, contact your eye doctor immediately.
4/23/15
 Susan DeRemer, CFRE
Susan DeRemer, CFRE
Vice President of Development
Discovery Eye Foundation