The Difference Between an Optometrist and an Ophthalmologist
The Difference Between an Optometrist and an Ophthalmologist
There are a number of players on your eye-health team, among them your optometrist and your ophthalmologist. It’s not always obvious, however, what position each plays and when you should call on which professional.
Optometrists
An optometrist holds a doctor of optometry (OD) degree. An optometrist generally completes a four-year college program in the sciences, plus four years of postgraduate professional training in optometry school.
Optometrists examine eyes for vision and health problems, and correct refractive errors with glasses and contact lenses. Some optometrists also provide low vision care and vision therapy. In the United States, optometrists may prescribe medications to treat certain eye problems and diseases, and their scope of care can differ by state. While not licensed to perform eye surgery, optometrists can play a role in pre- and post-operative care, if you have eye surgery performed by an ophthalmologist.
Ophthalmologists
An ophthalmologist is a medical doctor (MD) or a doctor of osteopathic medicine (DO), who specializes in eye and vision care. Ophthalmologists complete four years of college, four years of medical school, one year of internship and at least three years of residency in ophthalmology. Some ophthalmologists also have one or two years of additional training to become specialists in cornea, retina, glaucoma, oculoplastics, pediatrics or neuro-ophthalmology.
Ophthalmologists perform eye exams, diagnose and treat diseases, prescribe medications and perform eye surgery. They also prescribe corrective lenses.
Which one do I call?
Both optometrists and ophthalmologists perform routine eye exams, and are both trained to detect, diagnose and manage eye diseases. Both can prescribe corrective lenses, and both must fulfill continuing education requirements to maintain their licenses.
If your eyes are healthy, which type of professional to see is a matter of personal preference. If you already have a medical eye problem, such as diabetes, or a family history of AMD or glaucoma, you should consider seeing an ophthalmologist. While most optometrists offer medical treatment for common eye problems and chronic eye diseases, such as pink eye, dry eye or allergies, certain eye disorders require treatment by an ophthalmologist, particularly if you need surgery, laser therapy or other specialized care.
In some cases, your optometrist and ophthalmologist may work as a team. In such a setup, the optometrist is the equivalent of your primary-care doctor, who monitors your ongoing condition and care, and the ophthalmologist is your specialist, who manages your condition medically and/or performs surgery. For routine care, you may want to check with your insurance provider to see which, if either, professional they cover and for what services.



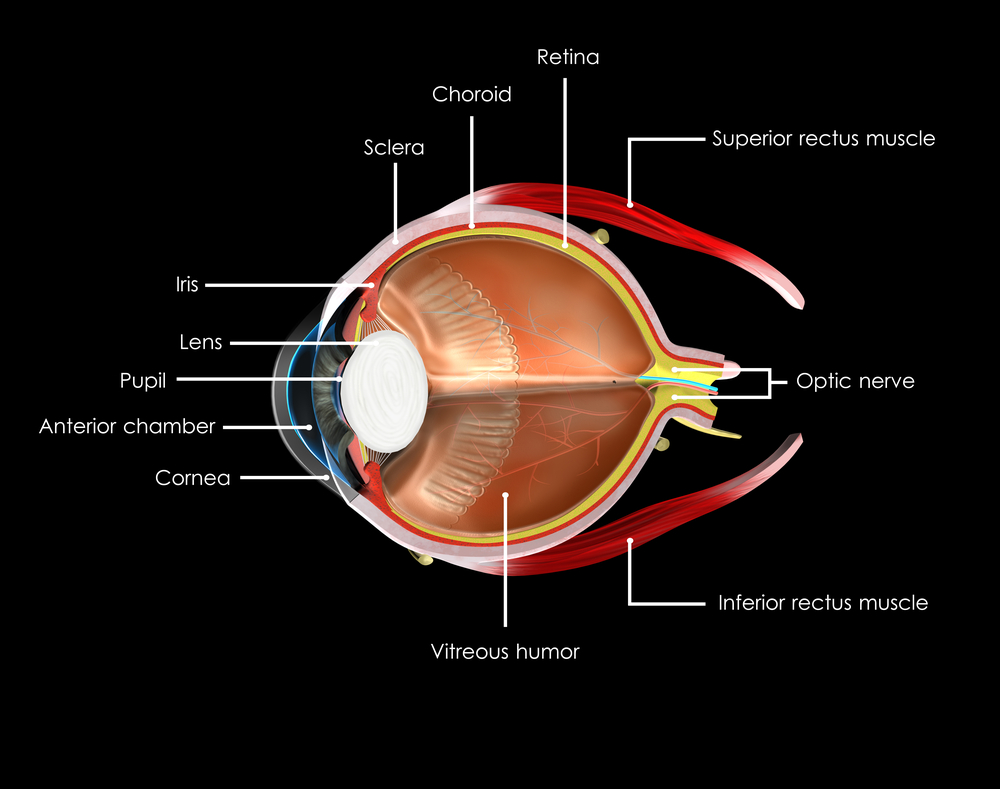
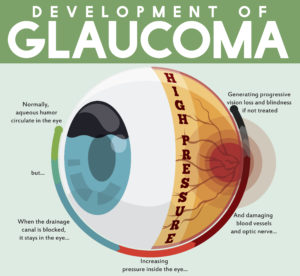 tic nerve, a part of the central nervous system that carries visual information from the eye to the brain.
tic nerve, a part of the central nervous system that carries visual information from the eye to the brain.