8/21/14
In the third of this series, Buddy Russell, from the Emory University Eye Center, provides a great overview of common pediatric eye diseases.
Some Conditions Frequently Seen in Pediatrics
A basic understanding of some of the conditions that may be present in pediatric patients is important to not only know what they are but also understand well enough to explain to the parent or caregiver. The following is intended to be an overview of some of those conditions and not a complete explanation.
- Nystagmus – Nystagmus is a vision condition in which the eyes make repetitive, uncontrolled movements, often resulting in reduced vision. These involuntary eye movements can occur from side to side, up and down, or in a circular pattern. As a result, both eyes are unable to hold steady on objects being viewed. Unusual head positions and head nodding in an attempt to compensate for the condition may accompany nystagmus. Most individuals with nystagmus can reduce the severity of their uncontrolled eye movements and improve vision by positioning their eyes to look to one side. This is called the “null point” where the least amount of nystagmus is evident. To accomplish this they may need to adopt a specific head posture to make the best use of their vision. The direction of nystagmus is defined by the direction of its quick phase (e.g. a right-beating nystagmus is characterized by a rightward-moving quick phase, and a left-beating nystagmus by a leftward-moving quick phase). The oscillations may occur in the vertical, horizontal or torsional planes, or in any combination. The resulting nystagmus is often named as a gross description of the movement, e.g. downbeat nystagmus, upbeat nystagmus, seesaw nystagmus, periodic alternating nystagmus. Having nystagmus affects both vision and self-concept. Most people with nystagmus have some sort of vision limitations because the eyes continually sweep over what they are viewing, making it impossible to obtain a clear image. If a refractive error is found, contact lenses may be the most effective way of obtaining best-corrected vision.
- Strabismus – Strabismus is any misalignment of the eyes. It is estimated that 4% of the U.S. population has strabismus. Strabismus is most commonly described by the direction of the eye misalignment. Common types of strabismus are esotropia (turn in), exotropia (turn out), hypotropia (turn down), and hypertropia (turn up). Eye misalignment can cause amblyopia in children. When the eyes are oriented in different directions, the brain receives two different visual images. The brain will ignore the image from the misaligned eye to avoid double vision, resulting in poor vision development of that eye. Also, an eye that sees poorly tends to be misaligned. The goal of strabismus treatment is to improve eye alignment, which allows for better work together (binocular vision). Treatment may involve eyeglasses, contact lenses, eye exercises, prism, and / or eye muscle surgery.
- Amblyopia – Amblyopia, sometimes called a “lazy eye,” occurs when one or both eyes do not develop normal vision during early childhood. Babies are not born with 20/20 vision in each eye but must develop it between birth and 6-9 years of age by using each eye regularly with an identical focused image falling on the retina of each eye. If this does not occur in one or both eyes, vision will not develop properly. Instead, vision will be reduced and the affected eye(s) are said to be amblyopic. This common condition, affecting up to 4% of all children, should be diagnosed and treated during infancy or early childhood to obtain optimum three-dimensional vision and to prevent permanent vision loss. What causes amblyopia?
- Misaligned eyes (strabismus)
Misaligned eyes are the most common cause of amblyopia. When both eyes are not aimed in exactly the same direction, the developing brain “turns off” the image from the misaligned eye to avoid double vision and the child uses only the better eye — the dominant eye. If this persists for a period even as short as a few weeks, the eye will not connect properly to the visual cortex of the brain and amblyopia will result. - Unequal refractive error (anisometropia)
Unequal refractive error is an eye condition in which each eye has a different refractive error and therefore both eyes cannot be in focus at the same time. Amblyopia occurs when one eye (usually the eye with the greater refractive error) is out of focus because it is more nearsighted, farsighted or astigmatic than the other. Again, the brain “turns off” the image from the less focused eye and this eye will not develop normal vision. Because the eyes often look normal, this can be the most difficult type of amblyopia to detect and requires careful vision screening of acuity measurements at an early age. Treatment with glasses or contact lenses to correct the refractive error of both eyes, sometimes with part-time patching of the better seeing eye, is necessary in early childhood to correct the problem. - Obstruction of or cloudiness (deprivation)
Obstruction of or cloudiness in the normally clear eye tissues may also lead to amblyopia. Any disorder that prevents a clear image from being focused can block the formation of a clear image on the retina and lead to the development of amblyopia in a child. This often results in the most severe form of amblyopia. Examples of disorders that can interfere with getting a clear image on the retina are a cataract or cloudy lens inside the eye, a cloudy and or irregular shaped cornea, or a droopy upper eyelid (ptosis) or eyelid tumor.It is not easy to recognize amblyopia. A child may not be aware of having one normal eye and one with reduced vision. Unless the child has a misaligned eye or other obvious external abnormality, there is often no way for parents to tell that something is wrong. In addition, it is difficult to measure vision in very young children at an age in which treatment is most effective.To treat amblyopia, a child and their caregiver must be encouraged to use the weaker eye. This is usually accomplished by patching the stronger eye. This covering of the stronger eye with an adhesive patch, an cclude contact lens or temporary surgery often proves to be a frustrating and difficult therapy. Patching will often continue for weeks, months, or even years in order to restore normal or near normal vision and maintain the improvement in the amblyopic eye. Occasionally, blurring the vision in the good eye with eye drops or lenses to force the child to use the amblyopic eye treats amblyopia. In some cases, cataract surgery or glaucoma surgery might be necessary to treat form deprivation amblyopia. Patching may be required after surgery to improve vision, and glasses or contact lenses may be required to restore appropriate focusing.Surprising results from a nationwide clinical trial in 2005 show that many children age seven through 17 with amblyopia may benefit from treatments that are more commonly used on younger children.
Treatment improved the vision of many of the 507 older children with amblyopia studied at 49 eye centers. Previously, eye care professionals often thought that treating amblyopia in older children would be of little benefit. The study results, funded by the National Eye Institute (NEI), appear in the April issue of Archives of Ophthalmology.
- Misaligned eyes (strabismus)
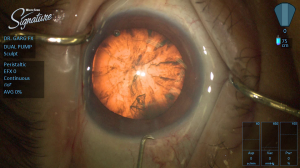
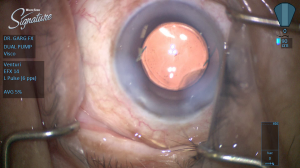
- Congenital Cataract – A congenital cataract, or clouding of the crystalline lens is present in 2-3 per 10,000 live births of children. The presence of a visually significant cataract in a child is considered an urgent disorder. The resultant form deprivation of vision requires immediate surgery to remove the obstruction, prompt optical correction and amblyopia therapy in unilateral cases. Until the 1970s, it was generally believed that there was no means of restoring the vision in an eye with a unilateral congenital cataract. However, subsequent studies demonstrated that excellent visual results could be obtained with early surgical treatment coupled with optical correction with a contact lens and patching therapy of the fellow eye. However, treatment results continue to be poor in some infants with unilateral congenital cataracts due to a delay in treatment or poor compliance with contact lens wear or patching therapy of the fellow eye. The Infant Aphakia Treatment Study (IATS) was designed to compare the visual outcomes in children 1 to 6 months of age with a unilateral congenital cataract randomized to optical aphakic correction with contact lenses or an intraocular lens (IOL). Children randomized to IOL treatment had their residual refractive error corrected with spectacles. Children randomized to no IOL had their aphakia treated with a contact lens. In previous publications we have shown that the visual results are comparable for these two treatments at 1 year of age, but significantly more of the infants randomized to IOL implantation required additional intraocular surgeries.
- Accommodative Esotropia – Accommodative esotropia refers to a crossing of the eyes caused by farsightedness. Accommodative esotropia is a type of strabismus. Children who are farsighted easily and automatically focus on objects at distance and near through accommodation. As a result, a child who is farsighted usually does not have blurred vision. However, in some children who are farsighted, this accommodative effort is associated with a reflex crossing of the eyes. Accommodative esotropia can begin anywhere from 4 months to 6 years of age. The usual age of onset is between 2 and 3 years of age.Full-time use of the appropriate hyperopic glasses prescription or contact lenses will often control the esotropia. When wearing the correction, the child will not need to accommodate and hence the associated eye-crossing reflex will disappear. However, after removing the prescribed correction, the crossing will reappear, perhaps even more than before the child began wearing the correction. Sometimes the correction will only cause the crossing to disappear when the child views a distant object. However, when gazing at near objects, crossing may persist despite the use of the correction. In these circumstances, a bifocal lens is often prescribed to permit the child to have straight eyes at all viewing distances. One potential advantage of contact lenses compared to spectacles when correcting hyperopic powers is the decrease in accommodative demand. The increased effort to converge the eyes with spectacles requires one to over come the resultant base out prism when viewing a near object.
 Buddy Russell, FCLSA, COMT
Buddy Russell, FCLSA, COMT
Associate, Specialty Contact Lens Service
Emory University Eye Center