6/5/14
Do you feel like your vision is getting worse? Do you feel like colors are not as vibrant as they used to be? Are you having more trouble with glare? If you have any of these symptoms, you may be experiencing the effects of cataracts.
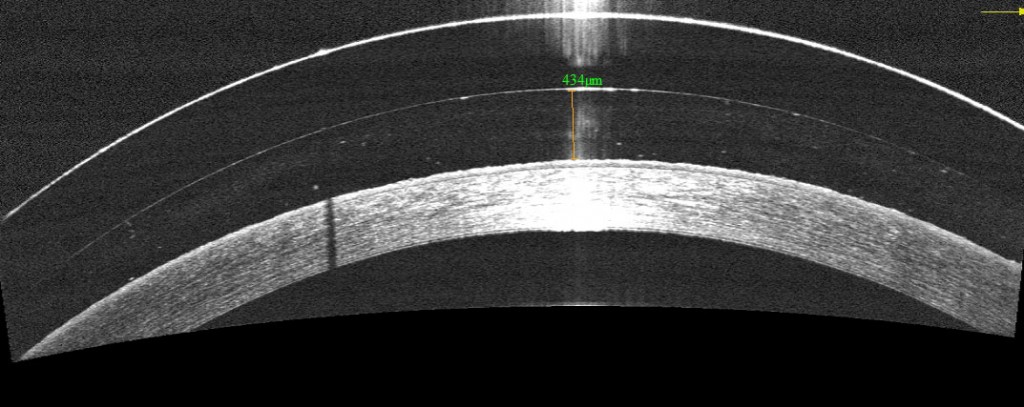
Cataracts are a normal aging process of the crystalline lens in the eye. Well you may ask — what is the crystalline lens? It is easiest to think of the eye as a camera. The eye has a lens (actually two) – the cornea (the front window of the eye) and the crystalline lens (inside the eye). It also has an aperture (the colored iris), and film (the retina). All these structures work together to focus light and allow us to see – just like a camera. When we are young (less than 40), the crystalline lens is flexible. This is why we are able to see distance and then near without the need for reading glasses. The crystalline lens is able to change its shape depending on where one is looking.

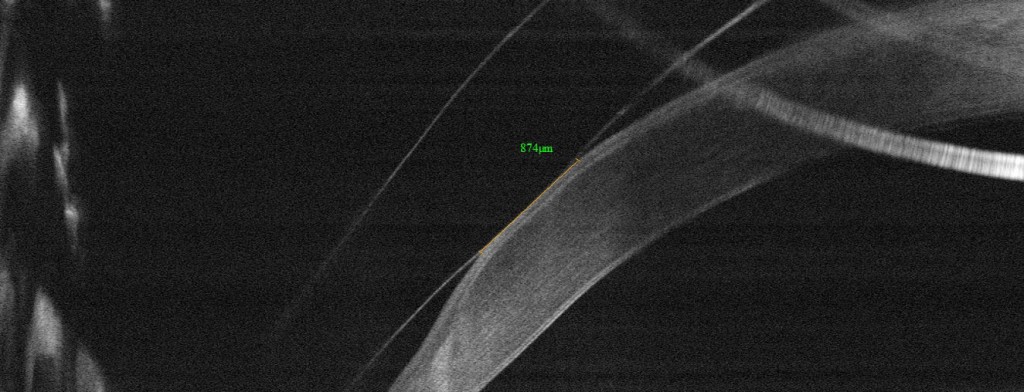
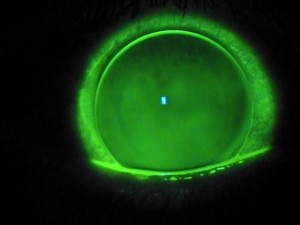
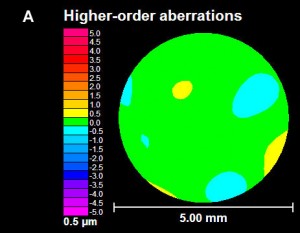
As we age, the crystalline lens becomes less flexible, thereby causing one’s near vision to be more blurry. This necessitates the need for reading glasses. As the crystalline lens become less flexible with age, the lens also starts to become more yellow and can also become cloudy. When the yellowing and/or clouding become visually significant, we refer to this as a cataract (figure 1).
Are cataracts dangerous? The simple answer is no. In the vast majority of cases, a cataract can be monitored until it becomes visually significant (drop in vision, glare, decreased contrast, vision related difficulties with day to day activities, etc). However, there are a few instances in which cataract removal is a medical necessity. Routine examinations by your eyecare provider can help you determine if you are at risk for these less common instances.
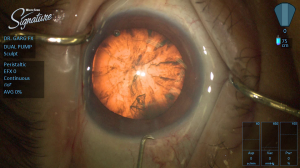
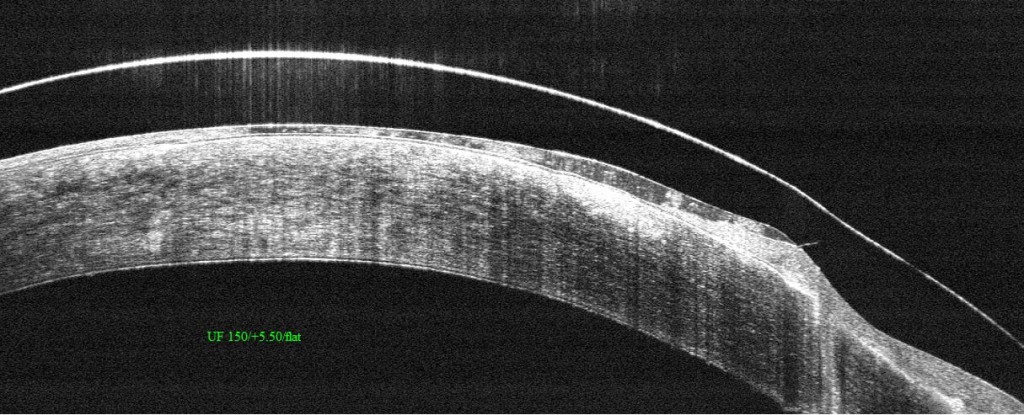
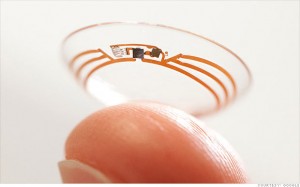
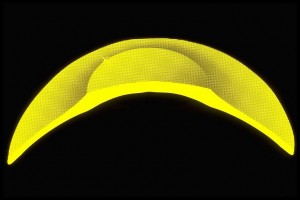
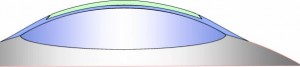
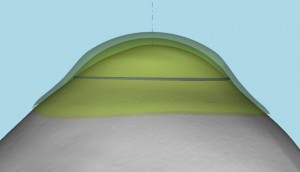
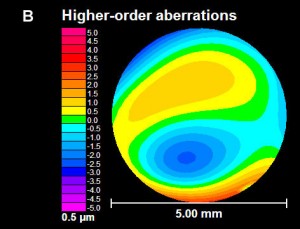
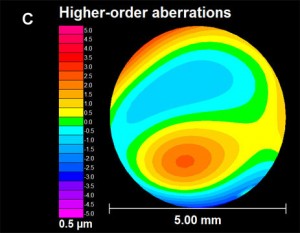
What can I expect during cataract surgery? Do you have to replace the crystalline lens with anything? Cataract surgery involves removing the clouded crystalline lens (figure 2) and replacing it with an artificial lens known as an intraocular lens (IOL) (figure 3). Surgery generally takes 10-15 minutes under a mild sedative, and you don’t have to stop any of your current medications. Anesthesia is achieved with drops and you will only feel mild pressure during the surgery. IOLs come in different styles – Standard IOLs grossly correct your vision and you can fine tune your vision (distance and near) with glasses post-operatively;
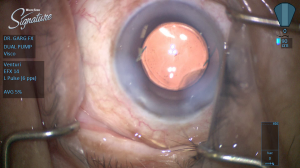
Toric (astigmatism correcting) IOLs allow for increased spectacle independence, but glasses will still be needed for distance or near; Accommodating IOLs “flex” within the eye to decrease your dependence on distance and near glasses; Multifocal IOLs allow spectacle independence for distance and near. I always counsel patients that there is no perfect IOL and you have to determine which IOL is best for your particular situation. Your doctor can help you decide which IOL is best for you. Generally, cataract surgery is extremely safe. Your doctor will discuss particular risks specific to your eye.
How do I know if cataract surgery is right for me? The best way to know if you have a cataract and if it time to consider surgery is to consult with your local ophthalmologist. If you have experienced a recent drop in vision, that is not correctable with glasses, cataract surgery may be able to restore your vision!
 Sumit “Sam“ Garg, MD
Sumit “Sam“ Garg, MD
Medical Director
Vice Chair of Clinical Ophthalmology
Assistant Professor of Ophthalmology
Gavin Herbert Eye Institute – UC, Irvine













 Bezalel Schendowich, OD
Bezalel Schendowich, OD
