6/3/14
What you need to know about eye drops.
Have you been staring at a computer all day and your eyes are tired? Have allergies been making your eyes watery and itchy? Are your contact lenses irritating your eyes? If you have experienced any of these conditions, you have probably turned to eye drops for relief.
While eye drops are an easy and effective means of treating a number of eye issues, there are many different eye drops available, both over the counter (OTC) and by prescription. It is wise to know what your underlying condition is before trying to get relief.

If your eyes are red and you may want to try a decongestant eye drop, which will shrink the tiny blood vessels in the “whites” of your eyes (sclera), but they also cause dryness so may not be a good choice if you wear contact lenses.
For lens wearers you are better off with a re-wetting drop to lubricate the eye and lens making you more comfortable. Another problem with the decongestant eye drops is over use – which can cause irritation and an increased tolerance that could lead to more redness.
If you suffer from allergies and antihistamine eye drop would be the best choice for relief from itchy, watery, red and swollen eyes. They work by reducing histamine in the eye tissue.
Lubricating eye drops, also known as artificial tears, are for short-term relief caused by temporary situations such as eye strain form computer use, being tired or being outdoors in windy and/or sunny conditions. If the condition is chronic, a prescription eye drop will be the best choice.
It is important to remember that if any of the above symptoms worsen or continue for an extended period of time, it is time to see your eye doctor to determine the underlying cause of your issue and to rule out eye disease. Postponing a visit could also lead to an eye infection.
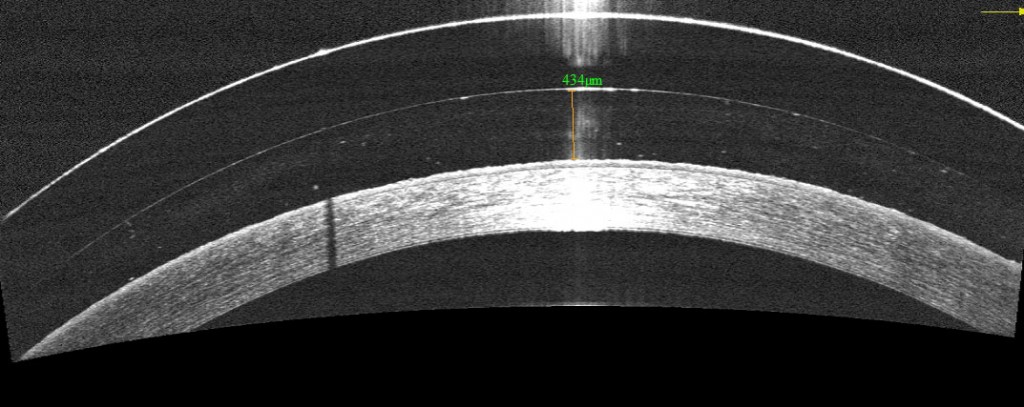
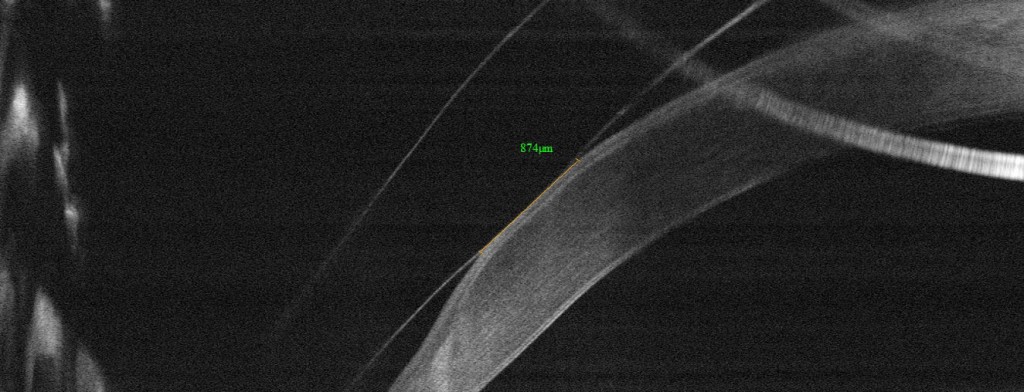
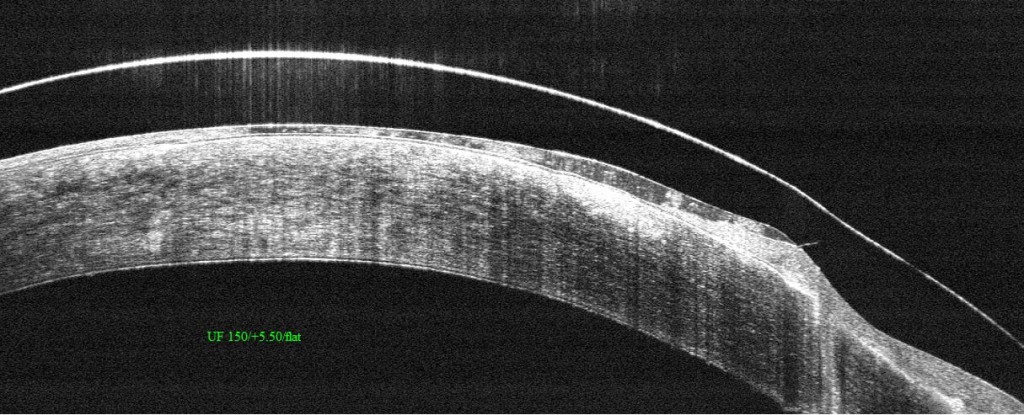
Prescription drops are used to treat a wide variety of eye diseases such as glaucoma, dry eye and the symptoms of ocular herpes. They are also used to help with healing from cataract surgery, corneal transplants, glaucoma surgery and even Lasik. it is extremely important to use them as often as your ophthalmologist recommends to improve healing and prevent infection.
Because of the ease of applying eye drops researchers are working toward using them to treat other eye diseases. Ocular herpes symptoms are sometimes treated with antiviral and steroid drops. But this only is targeted at the symptoms and not the underlying cause, the herpes simplex virus. Lbachir BenMohamed, PhD and Steven Wechsler, PhD at the University of California, Irvine, Gavin Herbert Eye Instittue have been working to determine what reactivate the herpes simplex virus and develop an eye drop that would either stop the reactivation of the virus or kill it.
Using eye drops to treat age-related macular degeneration (AMD) is also being explored. Researchers at the Institute of Ophthalmology at University College London are working with nanoparticles to deliver anti-VEGF drugs such as Lucentis and Avasitn to the back of the eye via drops. “The study shows that Avastin can be transported across the cells of the cornea into the back of the eye, where is stops blood vessels from leaking and forming new blood vessels, the basis for wet AMD.” While researchers in the Department of Ophthalmology, Tufts University School of Medicine in Boston “reported in their “proof of concept” study that topical application of a compound called PPADS inhibits damage to the tissues in the eye that impacts the individual’s ability to see color and fine detail, as well as reduces the growth of extraneous blood vessels in the back of the eye related to AMD.” It would work in both dry and wet AMD reduce the need for direct injections.
Eye drops, when properly applied, can provide temporary relief from symptoms of eye discomfort. But if the symptoms worsen or continue for an extended period of time, consult your eye doctor. To make sure you apply the eye drops correctly check out the article in our February 2013 newsletter for 12 easy steps to get the drops into your eyes and avoid infection.
One final note – keep your eye drops out of reach of children. Eye drops come in small bottles that are the perfect size for small hands and don’t have the same security tops found on other medications. The FDA has warned that ingredients found in some eye drops that relieve redness have caused abnormal heart rate, decreased breathing, sleepiness, vomiting and even comas in children five and younger that have ingested them. If you child has swallowed eye drops, call the Poison Help Line 800-222-1222.
 Susan DeRemer
Susan DeRemer
Vice President of Development
Discovery Eye Foundation