A symposium was held in Bethesda, Maryland at the National Institutes of Health on March 6, 2014. The purpose was to bring together clinicians and researchers from a wide variety of background to discuss the recently discovered differences in the function of the immune system in patients with age-related macular degeneration (AMD) and how it relates to aging. These differences are important to understand because they may lead to new therapeutic approaches to treat people which are high risk for AMD.
- Three researchers associated with the Discovery Eye Foundation attended the one-day conference. Cristina Kenney, MD, PhD, has worked in the field of AMD for over twelve years and is a leading expert on the genetics and molecular changes in the mitochondria as it related to the retinal cell death associated with AMD.
- Lbachir BenMohamed, PhD, is an expert immunologist with a tremendous understanding of how the immune system responds to infections and stress.
- Anthony Nesburn, MD, has been involved in AMD research at both the clinical and research levels.
By attending this meeting, all three researchers gained insight into the importance of the immune system with respect to maintaining a healthy retina and slowing the progression of AMD.
The highlights of the meeting were the following:
1. Emily Chew, MD (National Eye Institute) reviewed the clinical aspects of the disease stressing that there are many stages of AMD.
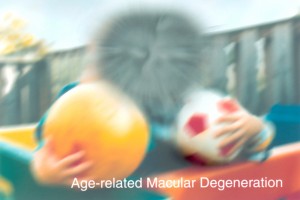
The early stage of AMD is diagnosed based upon the medium-size drusen (about the width of an average human hair) that can be seen underneath the retina. There may not be any visual changes in these patients.
The intermediate stage of AMD is when subjects have larger drusen and some degree of retinal pigment epithelial cell drop out. These patients may not have vision loss or other symptoms.
The late stages of AMD which can be categorized into the dry form (geographic atrophy) which has significant loss of the retinal pigment epithelial cells and overlying photoreceptor cells. Presently there in no treatment for this type of AMD.
These individuals can have changes that cause decreased vision. The second form of late AMD is the wet form (neovascular), which has growth of abnormal blood vessels beneath the retina that can cause significant loss of vision. The treatments for this type of AMD are anti-VEGF medications that block the growth of these vessels and help maintain good visual acuity.
2. Anand Swaroop, PhD (National Eye Institute) reviewed the genetics of AMD and summarized the work of numerous laboratories. It is now recognized that there are over 20 different genes associated with AMD. These genes fall into the categories of those involved with Complement Activation, Cholesterol Pathway, Angiogenesis, Extracellular Matrix and Signaling Pathways. Many of these genes have additive effects, meaning that if a patient has more than one high risk gene, then the likelihood of developing AMD increases. While we have learned a lot about the genes that are important, we still do not have any gene therapies that can be used to treat AMD.
3. Six different speakers presented their data related to animal models of AMD and it was agreed that there is not a “perfect” model because most of the animals do not have a macula, the region of the retina that is affected the most by AMD. However, there is still a lot to be learned by using the models that we do have because if we can better understand the basic pathways involved, then we can block or modify the pathways to prevent the damage.
4. Jayakrishna Ambati, PhD (University of Kentucky) presented data showing that there is a deficiency of an enzyme called DICER1 in the retinal pigment epithelial cells which leads to increased activation of inflammation via a protein complex called the inflammasome. He described some of the signaling pathways which are involved in the inflammasome activation. This is important because these pathways can become targets for treatment of the dry form of AMD.
5. Jae Jin Chae, PhD (National Human Genome Research Institute) also talked about the role that inflammation plays in the development of AMD. The data presented reviewed the pathways involved with activation of the inflammasomes which is the first step in a cascade of events that result in inflammatory diseases. They have identified a calcium-sensing receptor (CASR) which triggers the activation of the NLRP3, a key component of the inflammasome. Understanding how this series of events works allows researchers to develop medications to block or interfere with the pathway and therefore decrease the levels of inflammation.
 M. Cristina Kenney, MD, PhD
M. Cristina Kenney, MD, PhD
Professor and Director of Ophthalmology Research
School of Medicine, Dept. of Ophthalmology
University of California, Irvine