4/18/14
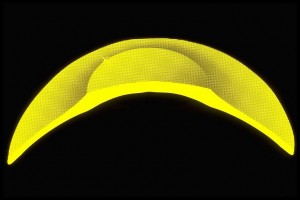
Keratoconus is a disease of the cornea in which the cornea loses its natural round shape and becomes distorted with cone-like bulging, progressive thinning, and associated reduction in vision quality. It is the front surface of the cornea that is the most significant focusing element of the eye. The irregularity of the front surface of the cornea in keratoconus is primarily responsible for the poor vision obtained with glasses since light that is focused through glasses lenses once again passes through air prior to reaching the corneal surface where again it is distorted. Contact lenses utilized for vision correction in keratoconus serve to “mask” the irregularity of the corneal surface thus creating a new smooth and regular front surface to the optical system.
Today contact lens correction for keratoconus is NOT synonymous with rigid corneal lenses. There are numerous options available to the contact lens specialist that can provide significant vision improvement for patients with keratoconus. It is the responsibility of the contact lens specialist to determine which design of contact lens is most appropriate for the individual patient. Let’s review the various options available today for the contact lens management of keratoconus.
Corneal rigid gas permeable contact lenses have been the mainstay for contact lens correction of keratoconus for many decades.
These are made of oxygen permeable rigid materials and are typically of a size that is smaller than the overall corneal diameter and they are fit to center as well as possible over the optical center of the cornea. Due to their rigid nature they do a wonderful job in masking the corneal irregularity and provide excellent vision. However, certain limitations have required us to develop other contact lens options for keratoconus. The limitations include; difficult initial adaptation and ongoing comfort issues for some patients, difficulty in centering over the optics of the eye in cases of more advanced and decentered cones, and occasional cases where lenses are not stable on the cornea and will dislocate. Most importantly, corneal rigid lenses that are fit “flat” and bear on the apex of the cone may induce progressive corneal scaring over time. Current fitting philosophy for these lenses attempts to fit with clearance over the cone apex.
Soft contact lenses have a significant role in the treatment of keratoconus. Mild and early cases can be managed with traditional non-specialty soft contact lenses as long as the degree of corneal distortion is not too severe.
Typically soft astigmatism correcting contact lenses are required. More advanced cases can be treated with specialty keratoconic designed soft lenses. These lenses typically have the central optic zone thickened in order to mask the corneal irregularity. However, the periphery of these lenses is thinned and provides excellent comfort and eye health response, especially when designed with highly oxygen permeable materials. We have been able to manage many cases of moderate and somewhat severe keratoconus with these specialty lenses. The advantage primarily is in lens wearing comfort and positional stability on the corneal surface. The limitation is typically if these lenses can provide adequate vision correction for the individual.
Piggyback or tandem lens systems utilize a combination of rigid corneal gas permeable lenses and soft lenses. Typically we utilize a thin, highly oxygen permeable soft disposable lens with insignificant power and then fit an appropriate gas permeable rigid lens on top of the soft disposable lens. The rigid lens provides the vision correction and the soft lens provides superior comfort compared to the rigid lens being fit directly on the eye surface and also occasionally helps with centration of the rigid lens over the optics.
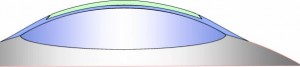
A variant of this system is called a “recessed pillow lens system” (RPLS) where a custom soft lens is created with a partial thickness cut out or recess that can hold a rigid lens in place. This can be used when a typical piggyback/tandem system cannot allow the rigid lens to center properly.
Hybrid contact lenses are available in specialty designs to address keratoconus. A hybrid lens is constructed with a rigid gas permeable lens center and a soft lens “skirt”. Again, the rigid lens provides the vision correction and the soft skirt provides excellent lens centration and improved comfort. Limitations of hybrid lenses include the inability to fit on more advanced and decentered cones and their potential to tighten up on the eye making removal more challenging and potential for eye irritation. However, new designs and fitting methods have addressed these issues in most cases.
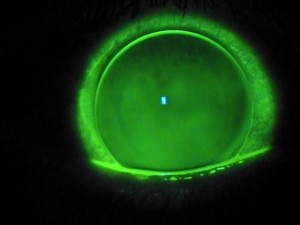
Finally, scleral lenses are an excellent option for keratoconus. These are large diameter rigid gas permeable lenses. They vault the entire cornea and do not touch the corneal surface at all.
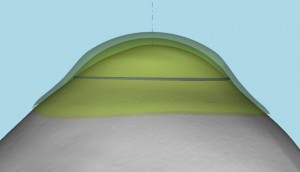
A tear layer is created below the scleral lens and the lens comes to rest gently on the white of the eye (the scleral surface). This results in very good lens comfort and it also protects the corneal surface from the negative effects of contact lens bearing. The rigid material provides excellent optics. Limitations of scleral lenses include the complexity of fitting, difficulty in insertion and removal on occasion and entrapment of mucous and debris below the lens requiring removal and rinsing of the lens for some patients. Overall scleral lens fitting is taking a larger role for keratoconus over the past few years. We are now developing totally customized scleral lens systems based on taking scans or impressions of the ocular surface to design a totally customized lens made uniquely for the individual eye that can address even the most distorted ocular surface.
Today we have multiple contact lens options to address the vision needs of our keratoconic patients. It is the responsibility of the contact lens practitioner to prescribe the most appropriate design for the individual patient.
 S. Barry Eiden, OD, FAAO
S. Barry Eiden, OD, FAAO
North Suburban Vision Consultants, Ltd., President and Medical Director
www.nsvc.com
National Keratoconus Institute, President and Medical Director
www.nkci.org
EyeVis Eye and Vision Research Institute
sbeiden@nsvc.com

