5/20/14
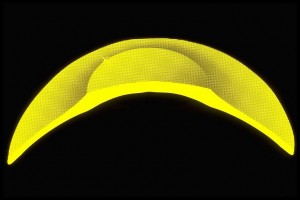
Summer vacation is around the corner and for children this means more time spent outside playing, swimming, or going to the beach. All of this outside activity increases their exposure to ultraviolet rays which is of particular concern because the lens of a child allows 70% more UV rays to reach the retina than in an adult. This may put them at increased risk of developing debilitating eye diseases such as cataracts or macular degeneration as adults.

If you are wearing sunglasses to combat the bright sunlight, then your child should be wearing them, from babies on up. Wrap-around sunglasses provide more sun and eye protection. Wearing protective goggles during sports activities is also important as the National Eye Institute reports there are more than 100,000 sports-related eye injuries every year with 42,000 requiring emergency care.
While it may be hard to get them to leave them on, or if they keep falling off, invest in a strap that can range from $4.50-$10.00. They can be made of neoprene with fun designs like Croakies or they can use an adjustable cord like Chums. In any case it also helps cut down on lost sunglasses.
Pediatricians offer the following five suggestions for children to enjoy a fun and safe summer:
1. Wear sunglasses – especially younger children
During our lives, almost half of the time we spend outdoors is before the age of 12. Sunglasses for children don’t have to be expensive, but make sure they are rated to block both UVA and UVB radiation. Glasses should also have a polycarbonate lens to withstand shattering.
2. Wear protective eye gear for ball or shooting sports
Every year there are 18,000 sports-related eye injuries in US hospital emergency rooms. The American Academy of Ophthalmology recommends that children wear polycarbonate goggles for baseball, basketball and racket sports, including tennis. It becomes even more important with shooting games like air-soft where the projectiles are so small, but can do major damage to the eye. Regular glasses are not recommended if they cannot be secured to the head or are not made from polycarbonate. Also make sure the goggles have proper sun protection for outside sports.
3. Don’t rub if sand gets in the eyes
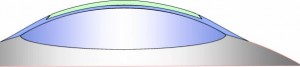
If a child gets sand into his eyes, take the child immediately to a sink with running water. Do not allow them to rub their eyes as this can scratch the outer layer of the eye known as the cornea. Use a clean cup to pour water over the eyes to remove sand. Encourage blinking and do not discourage crying, because tears remove eye irritants. If flushing and blinking does not work, seek immediate medical attention.
4. Use a non-irritating sunscreen
While you can use adult sunscreens for children, make sure it is PABA free, since that chemical can cause irritation in some people. If your child gets a rash from his sunscreen, review the ingredient’s list and choose a different one. UVA protection from titanium dioxide or zinc oxide tends to be less irritating than avobenzone, another common ingredient.
5. Wear a wide-brimmed hat
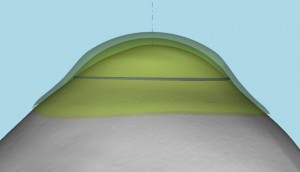
Don’t just rely on sunscreen. Have your child wear a hat with a wide brim. It not only provides additional protection against sunburn on susceptible areas like the nose, neck and ears, but it also helps to protect their eyes from harmful UV rays. Not all sunlight enters the eye direct from the front. Wrap-arounds may help protect light from coming in the sides, but they do not stop sunlight from coming in the top or reflective glare from coming up from the bottom.
6. Check chlorine levels in your pool
Too little chlorine in a swimming pool can allow algae and other bacteria to grow, which can lead to eye infections. On the other end of the spectrum, be sure to check the levels of chloramines and the pH of the pool to avoid stinging and redness. Swim goggles are helpful to keep pool water from entering the eye. If redness and irritation persist after swimming, it could be a sign of a more serious infection and medical attention is needed.
 Susan DeRemer, CFRE
Susan DeRemer, CFRE
Vice President of Development
Discovery Eye Foundation







![Mogk_Lylas_11C[1]](https://discoveryeye.org/wp-content/uploads/Mogk_Lylas_11C1.jpg)