6/26/14
Can dinner really be delicious medicine for our eyes?
Recent studies have shown compelling evidence that specific nutrients support eye health.* When a vitamin or mineral is given as a supplement, are there the supporting micronutrients and enzymes required for optimal utilization of that supplement by our bodies? Is a nutrient more bioavailable and/or more beneficial to our health as a foodstuff than as a supplement? Are there unintended effects from supplements that are not present when the nutrient is derived from a food source?**
Despite the many thought provoking questions, I personally take supplements as I feel it is difficult to acquire the nutrients strictly through food. Dietary preferences and requirements influence our everyday food choices as well as the quality of food available at our local grocery stores. Thoughtfully designed, well-sourced supplements have been shown to enhance eye health and general well being.
Here are some key nutritional principles which should be kept in mind to maximize the nutrient availability to our eyes and bodies from the foods that we eat:
1. Bioavailability: Vitamins A, D, E and K are fat soluble; the vitamin B-complex and vitamin C are water soluble. Dietary fats aid in the transport of fat soluble vitamins. Of particular importance to eye health are the fat soluble carotenoids in the vitamin A family, lutein and zeaxanthin. Carotenoids are the red, orange and yellow pigments found in fruit and vegetables such as kale, spinach, corn, apricots and orange bell peppers. To maximize their nutritional benefit, combine foods rich in carotenoids with a healthy source of fat such as olive oil, avocados or walnuts. Egg yolk contains the most bioavailable source of lutein and zeaxanthin and is preferentially deposited in the macula.
2. Nutrient Synergy: Nutrient synergy is the interaction of two or more nutrients that work together to achieve a greater effect than a single nutrient alone could. Foods have a vast array of micronutrients. We know that spinach contains a high level of lutein; however, we don’t know precisely how all the nutrients in spinach work together to promote eye health. Epidemiological studies show people who eat spinach have a lower risk for developing Age-related Macular Degeneration (AMD). Levels of lutein and zeaxanthin in the macula can be measured and low levels are a predictor for the risk of developing AMD.
3. Growing and Feeding Practices: The growing and feeding practices of the agriculture industry affect the nutrient profile and nutrient density of our food. Grass-fed versus corn-based animal husbandry, and wild versus farm-raised fish, alters the fatty acid profile. The amount of omega-3 fatty acids found in eggs varies depending upon the chicken’s diet. Ketchup from organically grown tomatoes contains nearly 50% more lycopene than from conventionally grown tomatoes. Choose quality ingredients whenever possible.
4. Cooking Techniques: Steaming, sautéing or pureeing will break down the plant cell walls increasing the body’s access to the lutein found in dark leafy greens. Cooking tomatoes will increase the availability of lycopene. Heat, however, diminishes the amount of vitamin C present. To maximize lutein and vitamin C, consume both fresh and cooked vegetable sources. Excessive heat and lengthy cooking times diminish vitamin content (mineral content will remain intact, however).
5. Whole Foods: Whole foods have benefits such as soluble and insoluble fiber which help to regulate blood sugar. Foods high in fiber have been shown to decrease total cholesterol, triglycerides and VLDL levels. Fiber supports gut health which is integral to nutrient absorption.
6. Select Eye Nutrient Dense Foods: Studies have highlighted lutein+zeaxanthin, the omega-3 fatty acids balanced with omega-6 fatty acids, the vitamin A family, the antioxidant vitamins C and E, as well as the mineral zinc. There a number of other nutrients that play a role in eye health including B vitamins, selenium and other plant based antioxidants. Knowing the food sources of these important nutrients will help you to make better food choices for eye health.
How does this sound for dinner tonight? Grilled wild salmon on a bed of lightly sautéed spinach with caramelized onions!
* AREDS 1, 2; LAST: Lutein Antioxidant Supplement Trial; ZVF: Zeaxanthin and Visual Function
** CARET: Carotene and Retinal Efficacy Trial
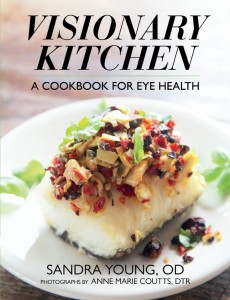
 Sandra Young, OD
Sandra Young, OD
Author of the award winning Visionary Kitchen: A Cookbook for Eye Health
www.visionarykitchen.com