8/5/14
For something different, and a little fun, here some interesting facts about animal eyes that you may not have known.
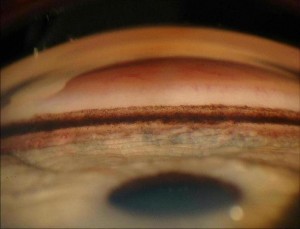
- Shark corneas are similar to human corneas, which is why they have been used in human transplants.
- A worm has no eyes at all.
- An owl can see a moving mouse more than 150 feet away.
- Guinea pigs are born with their eyes open!
- Scorpions can have as many as 12 eyes, but the box jellyfish has 24!
- Camels have three eyelids! This is to protect their eyes from sand blowing in the desert.
- Most hamsters only blink one eye at a time.
- Owls are the only bird which can see the color blue.
- Goats have rectangular pupils to give them a wide field of vision.
- A scallop has around 100 eyes around the edge of its shell to detect predators.
- Snakes have two sets of eyes – one set used to see, and the other to detect heat and movement. They also don’t have eyelids, just a thin membrane covering the eye.
- The four-eyed fish can see both above and below water at the same time.
- Owls cannot move their eyeballs – which has led to the distinctive way they turn their heads almost all the way around.
- A dragonfly has 30,000 lenses in its eyes, assisting them with motion detection and making them very difficult for predators to kill.
- Dolphins sleep with one eye open.
- The largest eye on the planet belongs to the Colossal Squid, and measures around 27cm across.
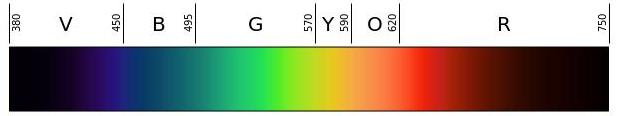
- Geckos can see colors around 350 times better than a human, even in dim lighting.
- The eyes of a chameleon are independent from each other, allowing it to look in two different directions at once.
- A camel’s eyelashes can measure up to 10cm long, to protect its eyelashes from blowing sand and debris in the desert.
- An ostrich’s eye is bigger than its brain.
- Dogs can’t distinguish between red and green.
- Polar bears have a third eyelid that helps filter UV light.
- Human eyes are not the most highly evolved. The mantis shrimp has four times as many color receptors as the human eye and some can see ultraviolet light.
- Pigeons can see millions of different hues, and have better color vision than most animals on earth.
- Cat’s eyes have almost 285 degrees of sight in three dimensions – ideal peripheral vision for hunting.
- Although color blind, cuttlefish can perceive light polarization, which enhances their perception of contrast.
- A moth’s eyes are covered with a water-repellant, anti-reflective coating.
- An ant only has two eyes, but each eye contains lots of smaller eyes, giving it a “compound eye.”
- Eagles have 1 million light-sensitive cells per square millimeter of the retina – humans only have 200,000.
- A honeybee’s eye is made of thousands of small lenses. A drone may have up to 8,600 and the queen be can have 3,000-4,000 lenses.
- The night vision of tigers is 6 times better than humans.
- Eyes on horses and zebras point sideways, giving them tremendous peripheral vision, to the point of almost being able to see behind them, but it also means they have a blind spot right in front of their noses.
 Susan DeRemer, CFRE
Susan DeRemer, CFRE
Vice President of Development
Discovery Eye Foundation