In this day and age of advancing technology, corneal transplants have changed from a long arduous ordeal to a more simple and precise procedure that offers faster visual recovery. Instead of replacing the entire cornea for any and all corneal diseases, we now perform disease targeted partial corneal transplants. If the disease involves the back layer of the cornea, we perform endothelial keratoplasty and replace only the diseased inner layer of the cornea. Conversely, if the problematic portions are the front layers of the cornea, we perform anterior lamellar keratoplasty. The co-morbidity and risk of rejection from partial corneal transplants are significantly less than the traditional full thickness transplants.
With endothelial keratoplasty, a small incision, about 4-5 mm is made and a sheet of donor endothelial cells are placed into the anterior chamber of the eye. A large air bubble is then used to float this sheet up so that it opposes the posterior or back portion of the cornea. The patient is asked to position face up for 24 hours. Over this period of time, the cells will “stick” on their own and thus no sutures are required to keep the graft in place.,/span> Anterior lamellar keratoplasty is done for superficial scars and opacities of the cornea or for keratoconus, a genetic degeneration of the cornea that is seen in younger individuals. In this case, the native endothelial cells of the patient are healthy and therefore are left intact while the remainder of the cornea is transplanted. This significantly lowers the risk of rejection, which is traditionally a much higher risk in young patients. Multiple sutures are required to maintain this graft in place however, with the advent of femtosecond laser technology, the wound configuration is made in such a way as to promote rapid healing and visual recovery. (Figure 1) Sutures are removed at an earlier time than with traditional surgery and the eye is able to undergo visual rehabilitation with glasses or contact lenses in 3-6 months’ time. Corneal transplantation does not require waiting on a list for a donor to become available like it once did. There are now multiple excellent eye banks across America that harvest, screen, and distribute donor tissue to surgeons. This way, tissue is readily available and patients only need to schedule a time based on their own and their surgeon’s time schedule. Post operatively, patients are asked to return to regular activity with the exception of no heavy lifting or bending for a period of 2 months. Antibiotic and anti-rejection drops are started immediately after surgery and continued for several months after. No oral medications aside from the patient’s regular medications are required.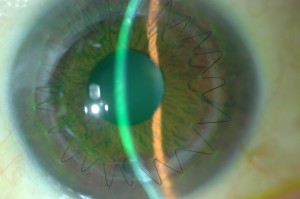
 Marjan Farid, MD
Marjan Farid, MD
Director of Cornea, Cataract, and Refractive Surgery
Vice-Chair of Ophthalmic Faculty
Director of the Cornea Fellowship Program
Associate Professor of Ophthalmology
Gavin Herbert Eye Institute, University of California, Irvine

