Scleral Contact Lenses have taken over a century to evolve into one of the best options for managing eye diseases such as keratoconus. This evolution began in the late 1800’s, with blown glass lenses. However, until the advent of highly oxygen permeable plastics, scleral lenses had very limited application. Now, with current technology and materials, scleral lenses have become a mainstream and rapidly growing lens option.
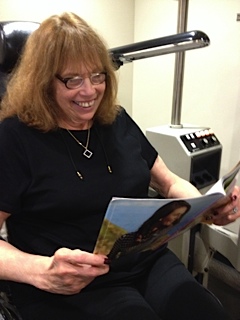
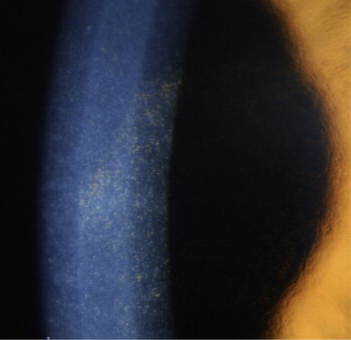
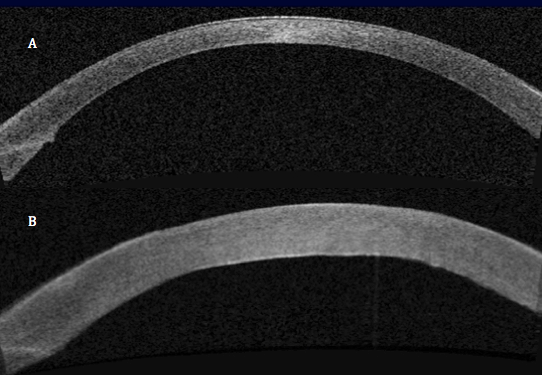
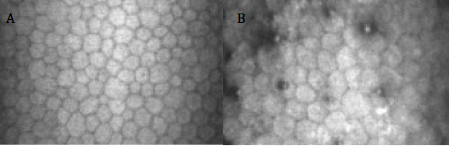
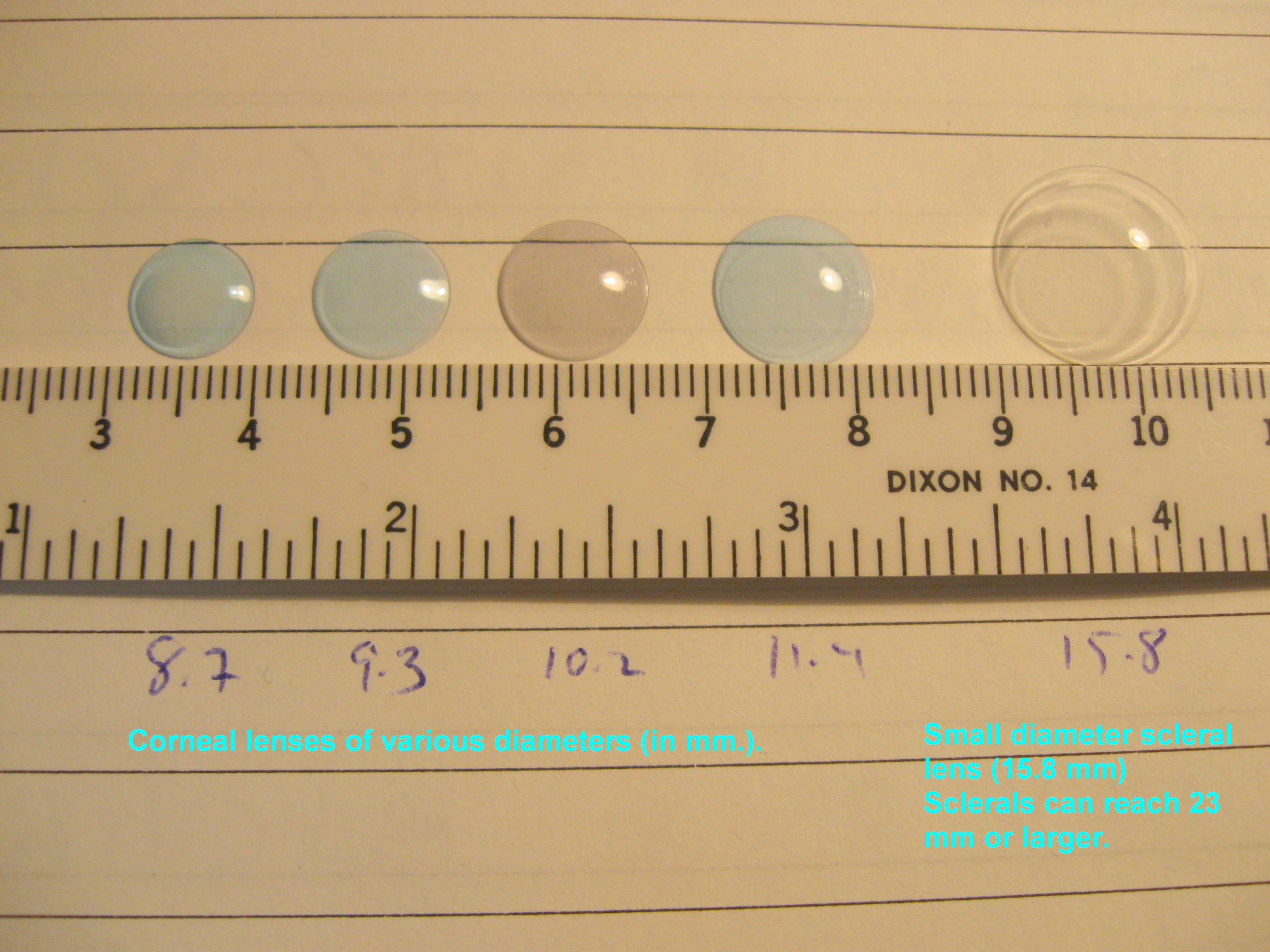
Scleral lenses are becoming more popular due to the exceptional comfort they can provide even to the most unusual eye shape. This comfort is attributable to their large size that allows them to tuck behind the eyelids, their relative lack of movement with eye blinks, and their fluid reservoir that keeps the cornea hydrated and does not actually touch the fragile corneal tissue in individuals with keratoconus.
As utilization of and demand for scleral lenses began to grow last decade, it became apparent that there was a need for more professionals trained in fitting scleral lenses, as well as someone to provide a consensus opinion for the eye care world on what the standard of care should be for these lenses. In addition, a process for providing a credential for those that attained a level of expertise in scleral lens fitting would allow those seeking experts in the field of fitting sclerals to find an experienced professional.
The Scleral Lens Education Society (SLS) was established in 2009 as an organization to help bring professional consensus to the suddenly rapidly growing area of scleral lenses. The mission statement of the SLS reads: “The Scleral Lens Education Society (SLS) is a non-profit organization 501(c)(3) committed to teaching contact lens practitioners the science and art of fitting all designs of scleral contact lenses for the purpose of managing corneal irregularity and ocular surface disease. SLS supports public education that highlights the benefits and availability of scleral contact lenses.”
Beginning with the founding board which included world renown experts in scleral lens fitting such as Greg DeNaeyer, OD, Christine Sindt, OD, and Bruce Baldwin, OD, PhD, the SLS has worked to spread the word about the potential benefits of scleral lens wear to both providers and patients alike. Professional education has included scleral lens webinars, workshops, and lecture series that are always standing room only events.
Currently, the SLS has over 2000 member contact lens practitioners as well as over 50 fellows, or certified scleral lens fitters that have demonstrated their expertise through a peer reviewed process of case reports, publications, and lectures. Many of these members and fellows are international, with SLS fellows from 11 countries, 5 different continents, and 20 different states in the US. Members hail from all 50 states, 6 continents, and over 40 countries.
In addition, the SLS has numerous industry sponsors that support the mission of the society to provide patient access to experienced fitters across the world. The sponsors provide the resources that allow the educational opportunities for practitioners as well as the website and patient resources that are available.
SLS board members are elected to serve in various capacities, including fellowship, public education, and international relations, and are elected to one year terms. The current board consists of:
President, Muriel Schornack, OD, Mayo Clinic, Rochester, MN
Vice President, Melissa Barnett, OD, University of California, Davis
Secretary, Michael Lipson, OD, University of Michigan
Treasurer, Mindy Toabe, OD, Metrohealth, Cleveland, OH
Immediate Past President, Jason Jedlicka, OD, Indiana University
Fellowship Chair, Pam Satjawatcharaphong, OD, University of California, Berkeley
Public Education Chair, Stephanie Woo, OD, Havasu Eye Center, Lake Havasu, AZ
International Chair, Langis Michaud, OD, University of Montreal
For more information about scleral lenses and the Scleral Lens Education Society, please visit the website at www.sclerallens.org. If you or someone you know might benefit from scleral lenses, you can locate a fitter in your area through the website as well. If you are unable to locate a fitter near you on the website, please contact the SLS and we will try to locate options in your local area.
7/2/15
 Jason Jedlicka, OD
Jason Jedlicka, OD
Clinical Associate Professor, Chief of Cornea and Contact Lens Service
Indiana University, School of Optometry