The following list of corneal transplant surgery terms is provided by the National Keratoconus Foundation (NKCF) website. They have more information on corneal transplants, as well as being a leader in information on keratoconus.
Corneal Transplant Surgery Terms Defined
Medical terminology is a language of its own. It can be confusing and alarming if you don’t know what the words mean. This will help you sort out the language of transplant surgery.

Atopic or Atopy – conditions associated with allergy like: asthma, eczema, hayfever
Decentration – off centered position
Donor tissue – the part of the cornea that is transplanted. The eye tissue removed upon a donor’s death for transplantation.
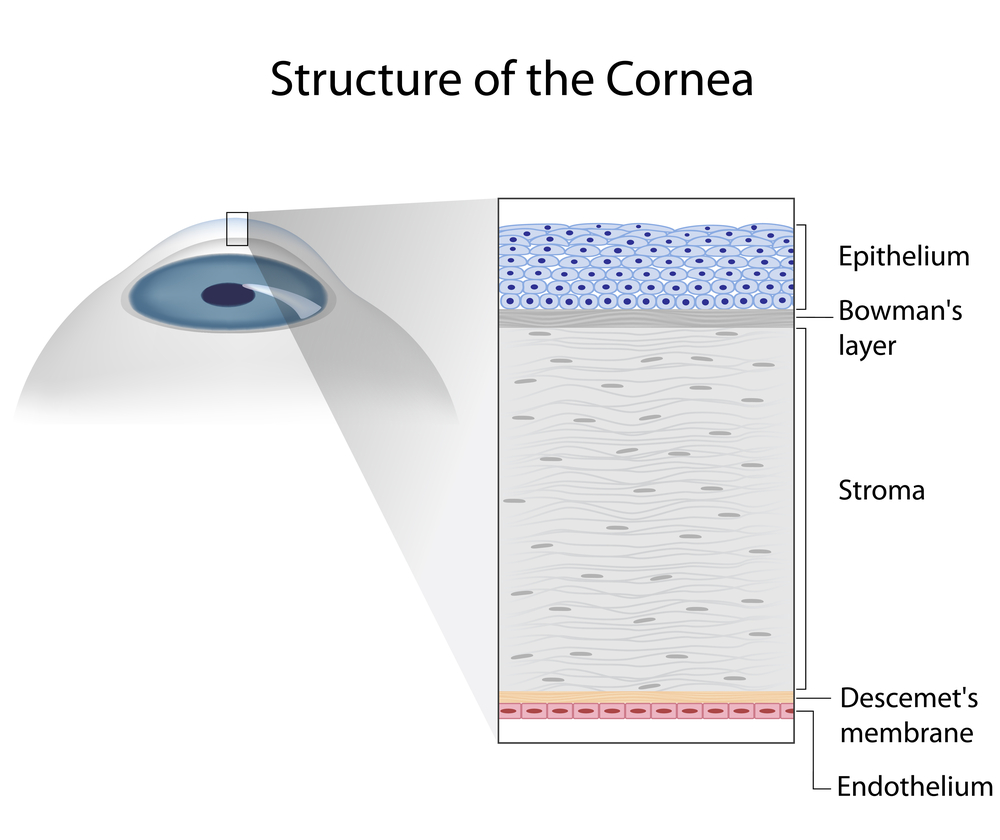
Epikeratophakia – a thin disk of donor cornea is sutured to the patient’s cornea after the patient’s epithelium (top layer) has been removed to add thickness.
Filaments – string or ribbon-like threads of epithelial cells and mucous that attach to the outer surface of the cornea.
Graft-host junction – where the donor cornea and patient’s cornea meet and are sutured.
Host tissue – cornea of the patient, the part of the patient’s cornea that is left in place when the central portion is removed to be replaced with the donor tissue.
Hydrops – a condition in which the back surface of a thin cornea ruptures, allowing fluid to waterlog the cornea, making it opaque instead of clear.
Keratic precipitates (KPs) – inflammatory cells that adhere to the innermost layer of the cornea and signal a rejection episode.
Kerato – (prefix) pertaining to the cornea
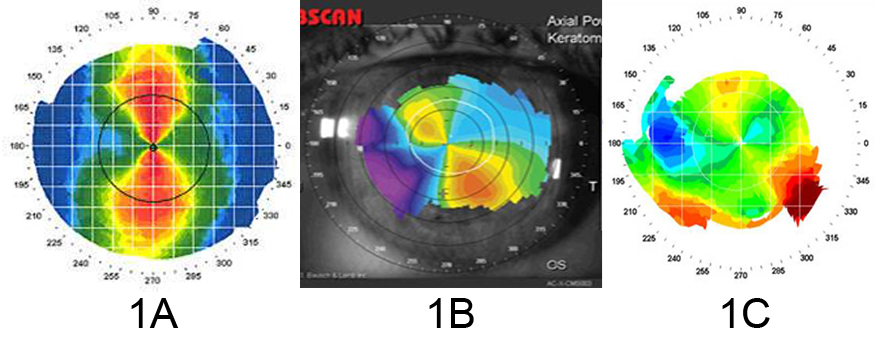
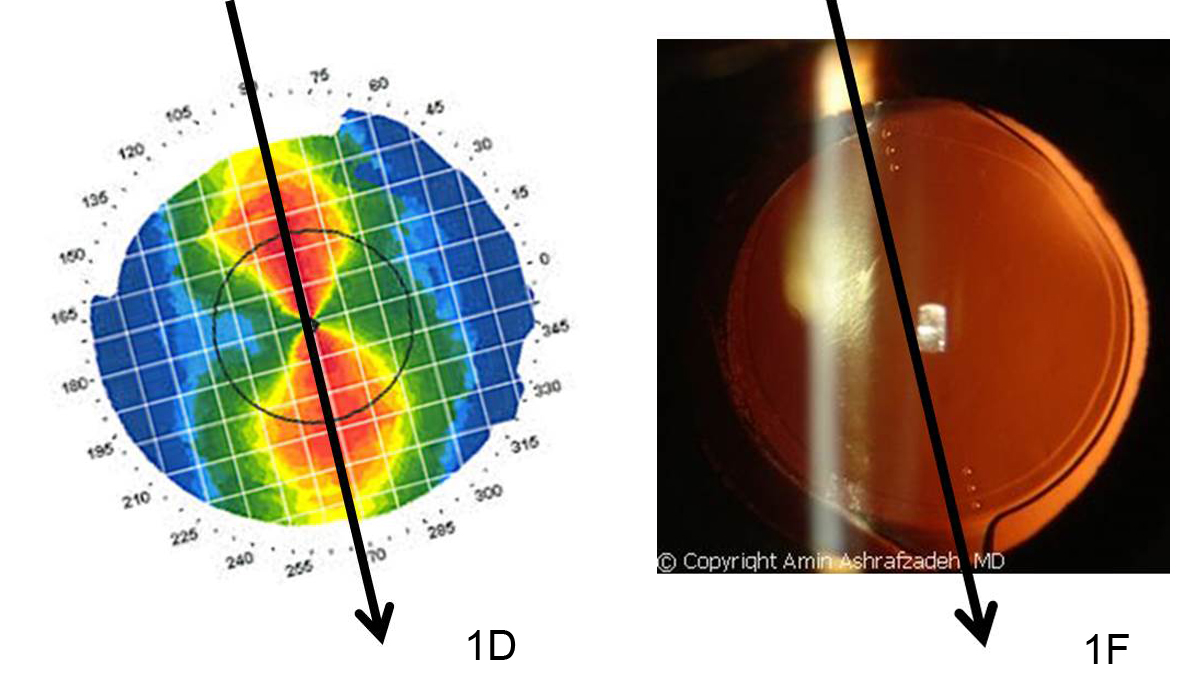
Keratometer – a device used to measure corneal curvature.
Keratomileusis – patient’s cornea is removed, frozen, reshaped on a computer assisted lathe- then returned to it’s original position.
Keratophakia – the surgical removal part of the surface of the cornea and its replacement with a donor cornea that is reshaped and transplanted to the patient’s cornea.
Keratoplasty – (corneal transplant) is the excision of all layers of the central portion of the cornea and replacement with a clear cornea from a human donor.
Lamellar Keratoplasty – (Non-Penetrating Keratoplasty) the outer two thirds of the cornea is removed and replaced with donor cornea.
LASIK – “laser assisted in situ keratomileusis.” It is a refractive surgery procedure for the correction vision in which a thin layer of the front of the cornea is lifted surgically and the underlying cornea is reshaped using an excimer laser. It is not a procedure applicable to keratoconus.
Penetrating Keratoplasty – (corneal transplant) full thickness layers of the cornea are replaced with a full thickness layer from a donor. The entire thickness of cornea is removed and replaced by full thickness donor corneal tissue.
Sutures – stitches, usually of a nylon material that are used to sew the new cornea tissue in place.
Trephine – a surgical instrument, a cutting tool, used to make a precise circular cut in tissue.
8/6/15
 Catherine Warren, RN
Catherine Warren, RN
Executive Director
National Keratoconus Foundation
A program of the Discovery Eye Foundation