Our bodies change as we age. Our metabolism slows down and we lose lean body mass. Changes occur in the kidneys, lungs, and liver. Total body fat typically increases. The digestive system slows down and changes, producing less of the fluids it needs to process food, thereby making it harder for the body to absorb important nutrients. We lose bone density, which can cause osteoporosis, fractures, and vertebral compression. Many of us lose some sense of taste and smell and our medications interfere with many vitamins. Because of these changes, older adults have very different nutritional needs than those who are younger. What is the best nutrition for older adults?

The basic challenge when one gets older is to meet the same nutrient needs as when we were younger, but doing it while consuming fewer calories. Extra weight and health issues may be the result if we don’t. We can meet the challenge by eating a healthy diet that provides the necessary nutrients and variables for good digestion and absorption of nutrients. A nutrient-dense (meaning foods high in nutrients in relation to their calories), fiber-filled, colorful and varied diet is key.
First, let’s look at some of the important vitamins and nutrients we need to insure healthy bodies:
WATER – of all the nutrients, this the most important. Drinking enough water reduces stress on kidney function, which can decline with age. It also eases constipation. Be aware that the ability to detect thirst declines with age. Instead of waiting to feel thirsty, drink water and other healthy fluids throughout the day. The goal should be about 8 glasses of water per day.
CALCIUM – Calcium’s most important role is for building and maintaining strong bones. Unfortunately, as we age, we tend to consume less in our diets. If you don’t get enough, your body will leach it out of your bones. If your diet includes dairy, three low-fat servings per day are recommended. But also consider plant alternatives such as collard greens, kale, and broccoli. In addition, tofu, almonds, sesame and chia seeds are other great non-dairy sources for calcium.
VITAMIN D – This vitamin helps the body absorb calcium, maintain bone density and prevent osteoporosis. Recent studies suggest it may also protect against some chronic diseases and vitamin D deficiency has been linked to an increased risk of falling in seniors. Vitamin D can be found in salmon, tuna, and eggs. You can also look for vitamin D fortified foods, including cereals, milk, some yogurts, and juices. Because aging skin becomes less efficient at producing the vitamin from sunlight, some experts believe seniors may need vitamin D supplements. You may want to discuss your vitamin D needs with your health care provider.
FIBER – Getting enough fiber in the diet will promote healthy digestion by moving foods though the digestive tract. It will also not interfere with the absorption of nutrients, which occurs with laxative use. Eating foods rich in fiber have additional benefits, including protecting against heart disease. So eat more whole grains, nuts, beans, fruits and vegetables.
POTASSIUM – Potassium is an essential mineral vital for cell function. It has been shown to reduce high blood pressure and the risk of kidney stones. It may also help keep bones strong. Older people can get the recommended daily amount by including fruits and/or vegetables in their diet at every meal. Banana, prunes, plums and potatoes with their skin are particularly potassium rich.
MAGNESIUM – Magnesium is important to many different physiological processes and keeps the immune system in good order. It also keeps the heart healthy and your bones strong. Absorption of magnesium decreases with age and some age-related medications, such as diuretics, may also reduce absorption levels. Eating as many unprocessed foods as possible, including fresh fruits, vegetables, nuts, seeds, grains, and beans will provide you a great source of magnesium.
VITAMIN B12 – Vitamin B12 is important in creating red blood cells and maintaining a healthy nerve function. Getting enough is the challenge for older people because of the decrease in absorption from food. The solution is to eat more food rich in B12 which includes fish, meat, poultry, eggs, and low-fat dairy. Also check with your health care provider about whether a supplement is in order.
FOLATE/FOLIC ACID – Anemia is the result of not enough of this essential B vitamin, which is related to B12 absorption and may improve hearing. Eat plenty of fruits and vegetables and/or make sure your breakfast cereals are fortified to ensure you are getting enough.
OMEGA-3 FATS – Primarily found in fish, these unsaturated fats have a wide range of benefits, including possibly reducing symptoms in rheumatoid arthritis and slowing the progression of age-related macular degeneration. They may also reduce the risk of Alzheimer’s disease and may even keep the brain sharper as we age. Strive toward at least two servings of fish a week and choose salmon, tuna, sardines, and mackerel which are especially high in omega-3. Plant sources of omega-3 include soybeans, walnuts, flaxseed, chia, hemp and sesame seeds, and cauliflower.
IRON – Iron intake sometimes appears to be low in many older adults. To improve absorption, include vitamin C-rich fruits and vegetables with iron-rich foods such as red meats, fish, and poultry.
ZINC – Along with vitamins C and E, lutein and zeaxanthin, it may help slow the progression of age-related macular degeneration. Eat lots of fruits and vegetables, especially those that are dark green, orange or yellow in color, such as kale, spinach, broccoli, peas, oranges, and cantaloupes.
VITAMIN E – This vitamin may have a potential role in the prevention of Alzheimer’s disease. Including whole grains, peanuts, nuts and seeds in your diet may help reduce the risk of this disease.
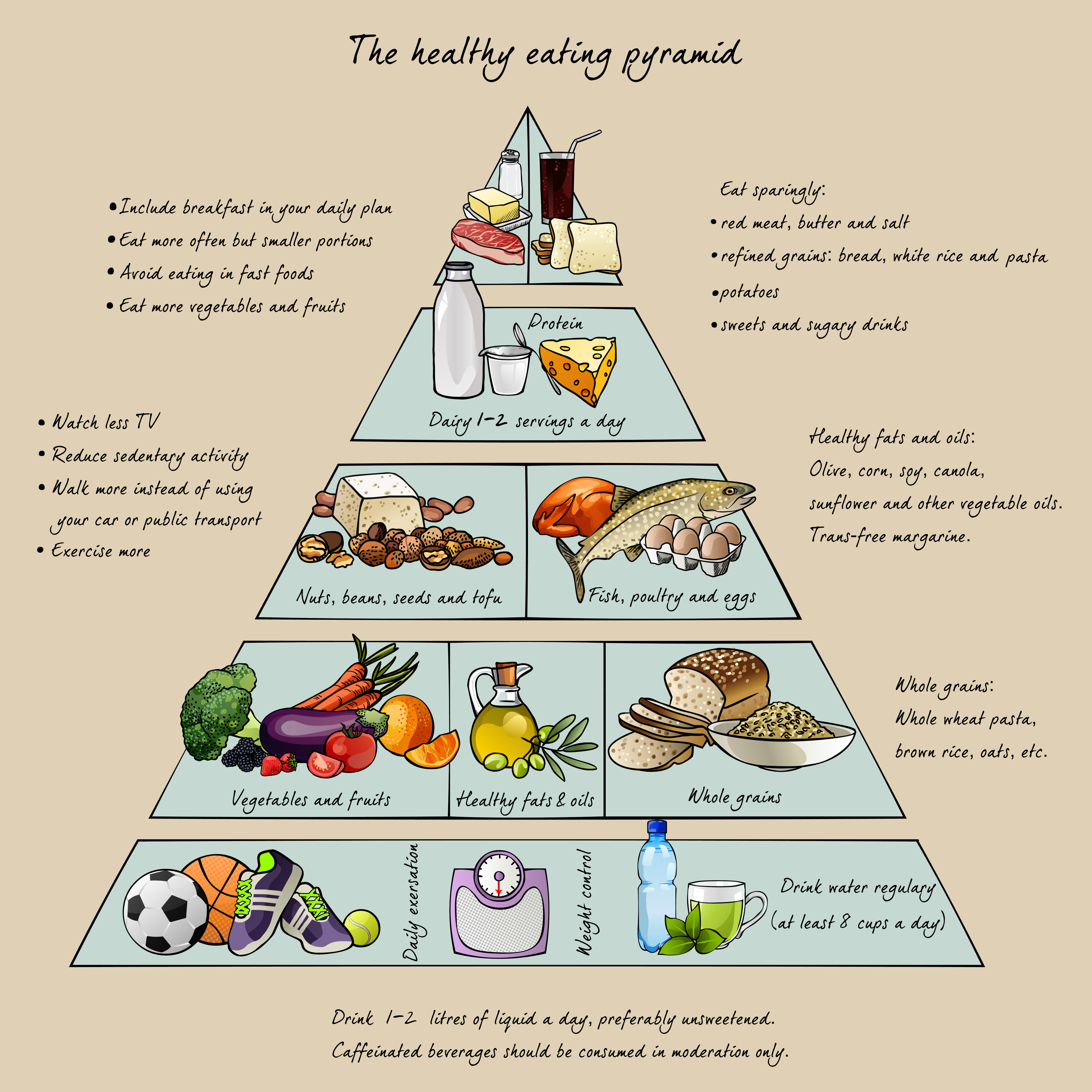
Now, how do we get these into our diet to ensure optimal nutrition? Strive to have your diet look like this:
- Colorful and varied. Have three to five different colors of food on your plate at each meal. This will translate into getting the most variety of nutrients. Eat more veggies than fruit.
- More natural and unprocessed. This will give you more fiber. Choose whole fruit over juice; whole grains over processed flours; include seeds, nuts, whole grains and beans in your salads and soups. Look at labels – choose foods with five or fewer ingredients you can pronounce.
- The majority of your food should be complex carbohydrate foods – vegetables, fruits, grain products, seeds, legumes and nuts. Choose more vegetables to keep the calorie count down.
- High-quality protein – eat less processed and high-fat choices and go for fish, lean meats, skinless poultry, low-fat dairy and plant-based protein sources.
- Less sodium, sugar, and “bad” carbs (such as white flour, refined sugars, and white rice). Too much of these things can lead to many age-related health issues and diseases.
- More steaming and sautéing and less battering and/or frying.
- Use of good fats such as olive oil, avocados, salmon, walnuts, flaxseed, and other monounsaturated fats to protect your body against heart disease.
- Try not to skip meals (it slows down your metabolism), eat smaller portions (we don’t need the extra calories), and exchange unhealthy snacks with healthier choices (raw veggies instead of potato chips, piece of fruit instead of a candy bar, etc).
- Lastly, don’t forget to drink your water!
2/10/15
 Michelle Moore, CHHC
Michelle Moore, CHHC
Natural Style Health