5/27/14
Last year Discovery Eye Foundation spoke to Dean Lloyd, who lost his sight to retinitis pigmentosa (RP), about his experiences with the Argus II “bionic eye.” After FDA approval, when the article came out, more people across the country have been fitted with the Argus II, using its 60-electrode system to help them regain some part of their vision. Researchers continue to try and improve upon the “bionic eye” such as this research for a 24-electrode version from Australia. Here is that article:

As one of only 30 people in the world with a “bionic retina,” Dean Lloyd has gained a bit of notoriety of late. The Argus II Retinal Prosthesis System received US market approval from the FDA on Feb. 14, and Lloyd has been part of the clinical trial since he was implanted with the device in 2007.
Lloyd’s vision difficulties began in the early 1960s, while he was in medical school at the University of South Dakota. He realized he wasn’t seeing the same thing as his classmates when looking through a high-powered microscope. He was misdiagnosed with Usher Syndrome, a rare genetic disorder that can result in deafness, blindness and dementia. While he was later correctly diagnosed with the less-dire x-linked retinitis pigmentosa (RP), he was asked to leave medical school due to his vision impairment.
“I had a moment of self-pity, then I needed to do some introspection to figure out how to find my future,” he says. “I decided I can’t give up on life. My brain works well … If your brain works, it can solve a lot of difficult problems. I realized I would survive.”
Seeing Stars
Armed with a BS in chemistry and an MS in bio-chemistry, Lloyd became a research chemist, then a software engineer. At the time, RP was having only one real effect on his life: reduced night vision. “I always thought people were seeing more stars than I saw. They’d see the big dipper and little dipper, and I didn’t see any dippers,” he recalls. Other than being extra-careful when driving at night, Lloyd’s daily life remained relatively unaffected until 1974, when he developed cataracts at age 34.
Lloyd’s wife decided she did not want to deal with any impact the disability would have on his ability to support their family. “She left and got the best divorce lawyers,” he says. “The court thought, because I was visually impaired, I wouldn’t be able to take care of my children. There were a lot of issues around disability and parent-ability in the mid- to late 70s.” Because of his vision loss, Lloyd lost custody of his two children. Believing disabled people were not treated fairly and seeing “the power of the court over people in their everyday lives,” Lloyd decided to go to law school. He passed the bar in 1982, “as a disabled person in a closed room,” and has been practicing law for more than 30 years.
He underwent two cataract surgeries, and a pair of convex lenses he wore on his nose was used in place of the actual lenses that had been removed from his eye. He had no difficulty with daytime mobility for nearly 14 years. But in 1989, he lost image formation. “I got an edema within the macula area, which didn’t go away,” he says. “I lost the ability to form images — that’s the point when you lose the opportunity for safe mobility.”
Lloyd had already been practicing law for seven years, and RP didn’t stop him. “I had quite a bit of experience in the courtroom,” he says. “I am fortunate to have a good memory, and I memorized everything I used there. I usually work with a junior or associate attorney; I do all the talking, and they handle all the documents and things. It didn’t change my career.”
A cane helped with his mobility, and for a few years, he says, “A doctor at Stanford pulled me in for some non-FDA experiments, because he knew I was a four-eyed guinea pig and was willing to try anything that might help RP.” None worked.
Lloyd was involved with several vision-related organizations and followed the progression of research and experiments to see if any might benefit him. In early 2007, he attended a Foundation Fighting Blindness meeting run by his daughter, who has “the recessive expression for RP.” The speaker that day was Dr. Jacque Duncan of UCSF, who interviewed all the attendees. Soon after, she contacted Lloyd to ask him to participate in the Argus II clinical trial.
He agreed immediately: “I figured if I lost the eye, I wouldn’t lose much, because it didn’t work anyway.”
The Bionic Retina
The Argus II Retinal Prosthesis System consists of three parts: an implant, glasses and a belt-worn video-processing unit (VPU).
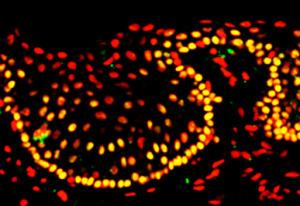
The implant is surgically implanted in and on the eye. It includes an antenna, an electronics case and an electrode array. The glasses contain a tiny video camera that captures a scene. The video is sent to the VPU, where it is processed and turned into electrical stimulations — instructions — that are sent back to the glasses through a cable. The glasses then transmit the instructions wirelessly to the implant antenna, which sends signals to the electrode array, which emits electric pulses. These pulses bypass damaged photoreceptors (RP damages photoreceptors and impedes image formation) and stimulate the retina’s remaining healthy cells, which transmit the information along the optic nerve to the brain. If all goes well, it creates the perception of patterns of light, which wearers can learn to interpret as visual patterns.
Chicken Dance
Duncan, working with another UCSF doctor, had Dr. Eugene de Juan put the Argus II implant in Lloyd’s right eye on July 17, 2007. A few weeks after an initial infection subsided, he did his first test walk with the device outside, looking for boundaries and points of light.
“Human eyes naturally move around, using a rapid ‘saccade’ movement,” Lloyd explains. “With the device, you have to physically move your head back and forth to find boundaries — like a chicken, which does not have moving eyes. They move their heads back and forth to see things. During my walk, the field-service worker would say, ‘Dean, Dean, more chicken movement.’”
After about a year and a half spending a half-day a week at UCSF for the trial, he had a second operation. “The device didn’t satisfy me,” he says. “I went through all that, and all I could see was a little point of light. Only nine of 60 electrodes were working. I said, ‘This isn’t going to cut it for me, because I want to see images.’ They reset the implant closer to the retinal tissue, and that dramatically improved the device.”
Lloyd conducted his own tests of the device at home. “I was one of first to use it to sort socks. I wear black socks to court and white socks to the gym. I went home after the implant and wanted to see how I could make it practically useful. So I went to my socks and found the device worked. I always got the white ones right!”
While he is generally pleased with the Argus II, the most he will say is, “It shows potential.”
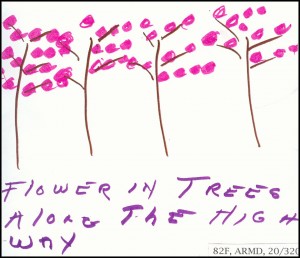
“The improvement was not very good at first. I wasn’t very impressed. There was a rumor going around that the implant restored vision. My vision wasn’t restored at all; I was not ascertaining images,” he says. “I do see boundaries. I can create an image. I know what a car should look like. I know what a tree should look like. I know what houses should look like. I know what objects should look like, and I have those images as memories in my brain. With this device, you can start to create an image by going back and forth, checking the boundaries and borders. We don’t have natural saccade movement helping us. The camera is right above my nose in a fixed position. It doesn’t move. You can create an image, but it takes a lot of time and a lot of work. It’s a labor-intensive task, and you have to have a good memory.”
The Argus II was approved by the FDA in February, and Lloyd is actively involved with Second Sight, the company that makes the device: “I am helping with new improvements,” he says. “I want this device to work. I didn’t go through all this for nothing.” He hopes an improved version will be approved this coming September, and he doesn’t rule out getting a new implant in the future if the improvements are worth it. To be honest, he says, “I find it annoying to move like a chicken.”
 Susan DeRemer, CFRE
Susan DeRemer, CFRE
Vice President of Development
Discovery Eye Foundation










![Mogk_Lylas_11C[1]](https://discoveryeye.org/wp-content/uploads/Mogk_Lylas_11C1.jpg)