The past year has taken a toll on the physical and mental health of millions of people. While we were rightly focused on slowing the spread of the pandemic, widespread shutdowns brought about a more sedentary, inactive lifestyle, which has led to increased weight gain and worsened mental health for many. As we look ahead and as more people receive the vaccine, it is time to start reprioritizing physical activity and placing much needed attention on our health.
The past year has taken a toll on the physical and mental health of millions of people. While we were rightly focused on slowing the spread of the pandemic, widespread shutdowns brought about a more sedentary, inactive lifestyle, which has led to increased weight gain and worsened mental health for many. As we look ahead and as more people receive the vaccine, it is time to start reprioritizing physical activity and placing much needed attention on our health.
It’s no secret that exercise is the best way to get in shape and to prevent serious health conditions, especially after this pandemic. But did you know that you can actually exercise your way to healthy eyes too? By eating a healthy diet and exercising regularly, you can help prevent eye conditions linked to obesity and being out of shape.
Below are a few tips on how to get your fitness regimen back on track.
- Set Goals – The first step to getting back in shape is deciding what you want to achieve. Take a personal inventory and write a contract with yourself, put it someplace where you can see it every day.
- Start Small – Getting too ambitious when planning goals can set you up for failure. Instead, ease into the changes. A lot of people get discouraged because they try to change their whole routine immediately.
- Build Momentum – Mini daily victories create a sense of accomplishment. A few daily successes will create a snowball effect. Add more challenges, then a few more and that’s what will keep the momentum going.
- Enjoy Your Workout – The best way to stick with an exercise routine, is enjoying it. You’re more likely to stay on schedule and exercise more often if you enjoy what you are doing. Hiking, swimming, boxing, dance or yoga are great options—and create atmosphere that’s inviting.
- Stretching Matters – It preps your muscles for exercise and cools them down after, guarding against injury. Stretching also improves your posture.
- Invest In Equipment – You don’t need to spend a lot of money—a few weights are enough to deliver results. Even minimal equipment allows for more intense and effective workouts.
- Make it a Habit – Exercise should be part of your daily routine, it should be as normal as showering or brushing your teeth.
- Get A Workout Buddy – If you can’t recruit a family member or friend, join a Zoom class or an outdoor club.
Stay active, get plenty of exercise and keep a healthy diet. When you’re tempted to slack off, or quit exercising all together—give yourself a day off to relax. Just remember how terrific you’ll look and feel when you keep moving.
You’ll probably agree it’s worth working out a few minutes each day to reap the rewards of good health and great vision!
Click here for Eye Healthy Recipes.





 Rest and blink your eyes – Researchers found that over 30% of people using digital devices rarely take time to rest their eyes. Just over 10% say they never take a break, even when working from home. The eye muscles get overworked and don’t get a chance to relax and recover. Experts suggest the 20-20-20 rule; every 20 minutes, focus your eyes and attention on something 20 feet away for 20 seconds. You can also get up and walk around for a few minutes.
Rest and blink your eyes – Researchers found that over 30% of people using digital devices rarely take time to rest their eyes. Just over 10% say they never take a break, even when working from home. The eye muscles get overworked and don’t get a chance to relax and recover. Experts suggest the 20-20-20 rule; every 20 minutes, focus your eyes and attention on something 20 feet away for 20 seconds. You can also get up and walk around for a few minutes. Reduce exposure to blue light – In the spectrum of light, blue is more high energy and close to ultraviolet light. So, if you use screens throughout the day, ask your eye doctor about the value of computer glasses that block blue light. Reducing exposure to blue light may help lessen vision problems. At home, using digital devices until bedtime can overstimulate your brain and make it more difficult to fall asleep. Eye doctors recommend no screen time at least one to two hours before going to sleep.
Reduce exposure to blue light – In the spectrum of light, blue is more high energy and close to ultraviolet light. So, if you use screens throughout the day, ask your eye doctor about the value of computer glasses that block blue light. Reducing exposure to blue light may help lessen vision problems. At home, using digital devices until bedtime can overstimulate your brain and make it more difficult to fall asleep. Eye doctors recommend no screen time at least one to two hours before going to sleep. Sit up straight – Proper posture is important. Your back should be straight and your feet on the floor while you work. Elevate your wrists slightly instead of resting them on the keyboard.
Sit up straight – Proper posture is important. Your back should be straight and your feet on the floor while you work. Elevate your wrists slightly instead of resting them on the keyboard. Set up monitor properly – Make sure your computer screen is about 25 inches, or an arm’s length, away from your face. The center of the screen should be about 10-15 degrees below eye level. Cut glare by using a matte screen filter. You can find them for all types of computers, phones, and tablets. Increase font size or set the magnification of the documents you are reading to a comfortable size.
Set up monitor properly – Make sure your computer screen is about 25 inches, or an arm’s length, away from your face. The center of the screen should be about 10-15 degrees below eye level. Cut glare by using a matte screen filter. You can find them for all types of computers, phones, and tablets. Increase font size or set the magnification of the documents you are reading to a comfortable size. Consider computer glasses –For the greatest comfort at your computer, you might benefit from having your eye doctor modify your eyeglasses prescription to create customized computer glasses. This is especially true if you normally wear distance contact lenses, which may also become dry and uncomfortable during extended screen time. Computer glasses also are a good choice if you wear bifocals or progressive lenses, because these lenses generally are not optimal for the distance to your computer screen.
Consider computer glasses –For the greatest comfort at your computer, you might benefit from having your eye doctor modify your eyeglasses prescription to create customized computer glasses. This is especially true if you normally wear distance contact lenses, which may also become dry and uncomfortable during extended screen time. Computer glasses also are a good choice if you wear bifocals or progressive lenses, because these lenses generally are not optimal for the distance to your computer screen. Get an Eye Exam – If you have tried all these tips and eye strain is still an issue, it might be time to see an eye care professional to schedule an eye exam. The exam may even detect underlying issues before they becomes worse.
Get an Eye Exam – If you have tried all these tips and eye strain is still an issue, it might be time to see an eye care professional to schedule an eye exam. The exam may even detect underlying issues before they becomes worse.
 Thanksgiving is almost here; a meal that nourishes the family bonds and traditions. It’s the one time of the year where you can guarantee your eyes will be bigger than your stomach.
Thanksgiving is almost here; a meal that nourishes the family bonds and traditions. It’s the one time of the year where you can guarantee your eyes will be bigger than your stomach.  Taking care of your health is critical and you may have concerns related to eye health as a result of the COVID-19 pandemic. The offices of Ophthalmologists and Optometrists are resuming the delivery of comprehensive eye and vision care and implementing new protocols to provide care in a safe and healthy environment.
Taking care of your health is critical and you may have concerns related to eye health as a result of the COVID-19 pandemic. The offices of Ophthalmologists and Optometrists are resuming the delivery of comprehensive eye and vision care and implementing new protocols to provide care in a safe and healthy environment.
 Tom Sullivan
Tom Sullivan
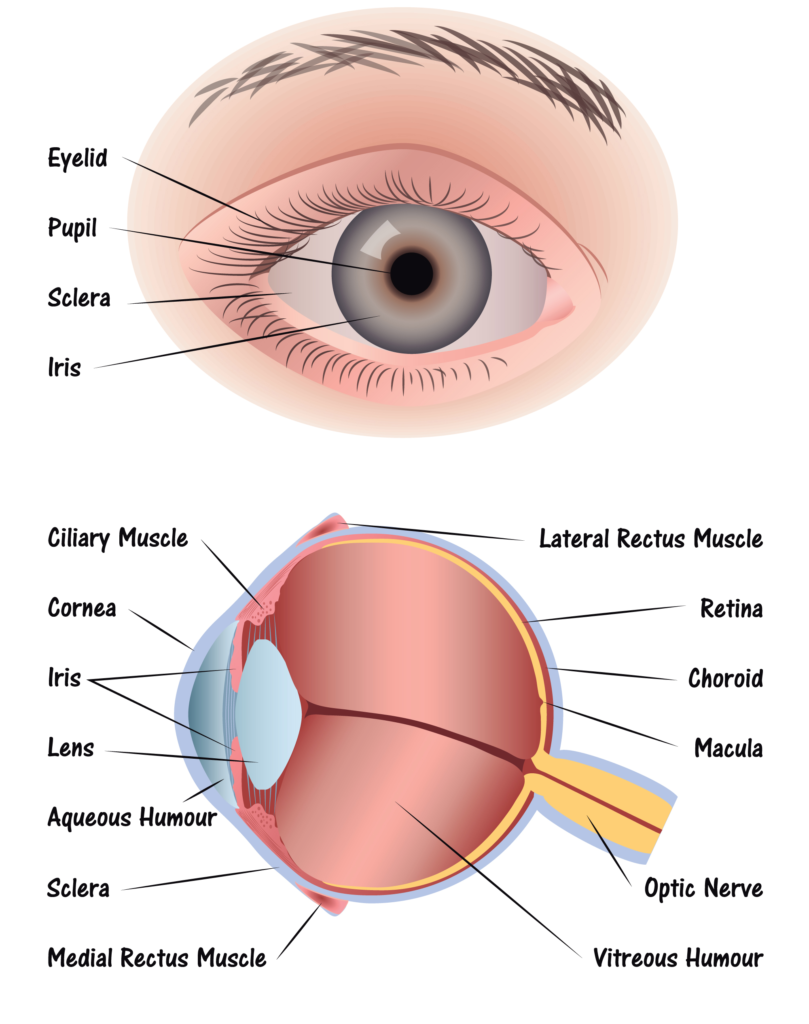 Step 1: Light passes through a thin layer of moisture
Step 1: Light passes through a thin layer of moisture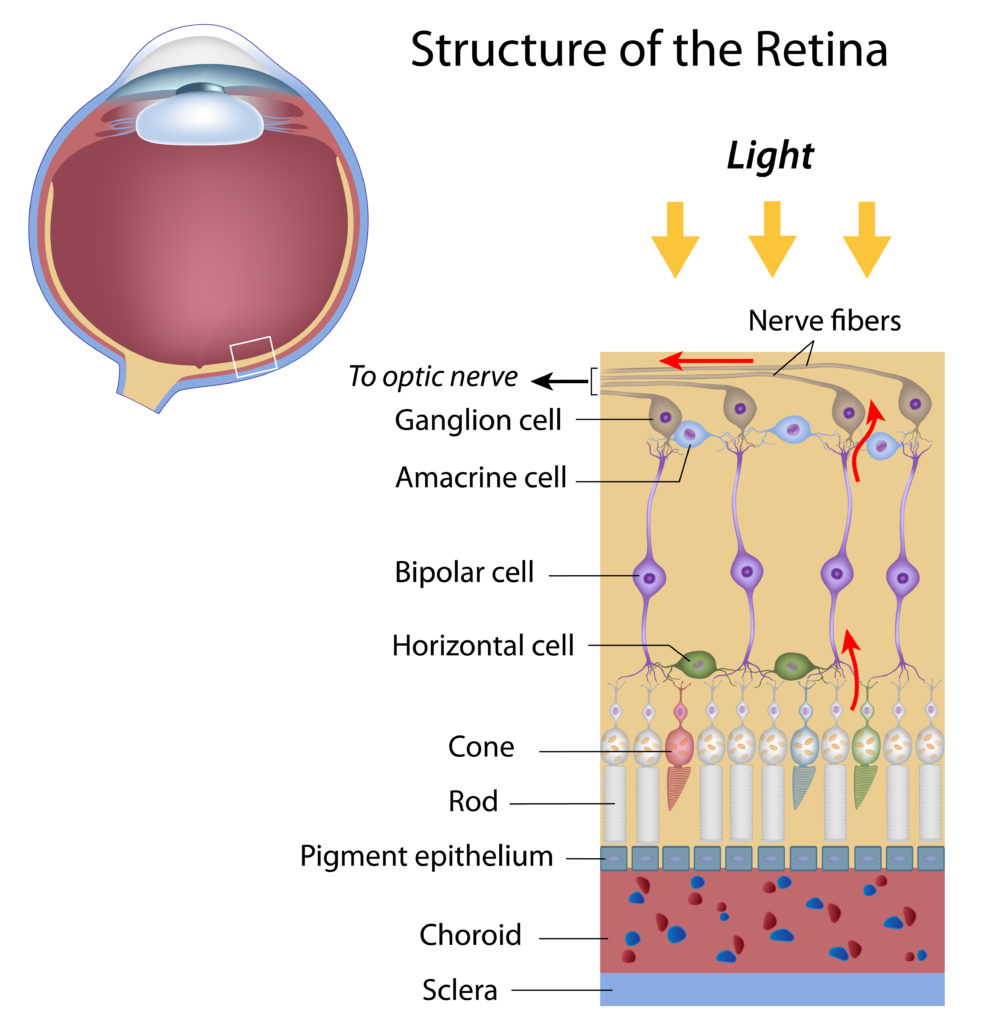
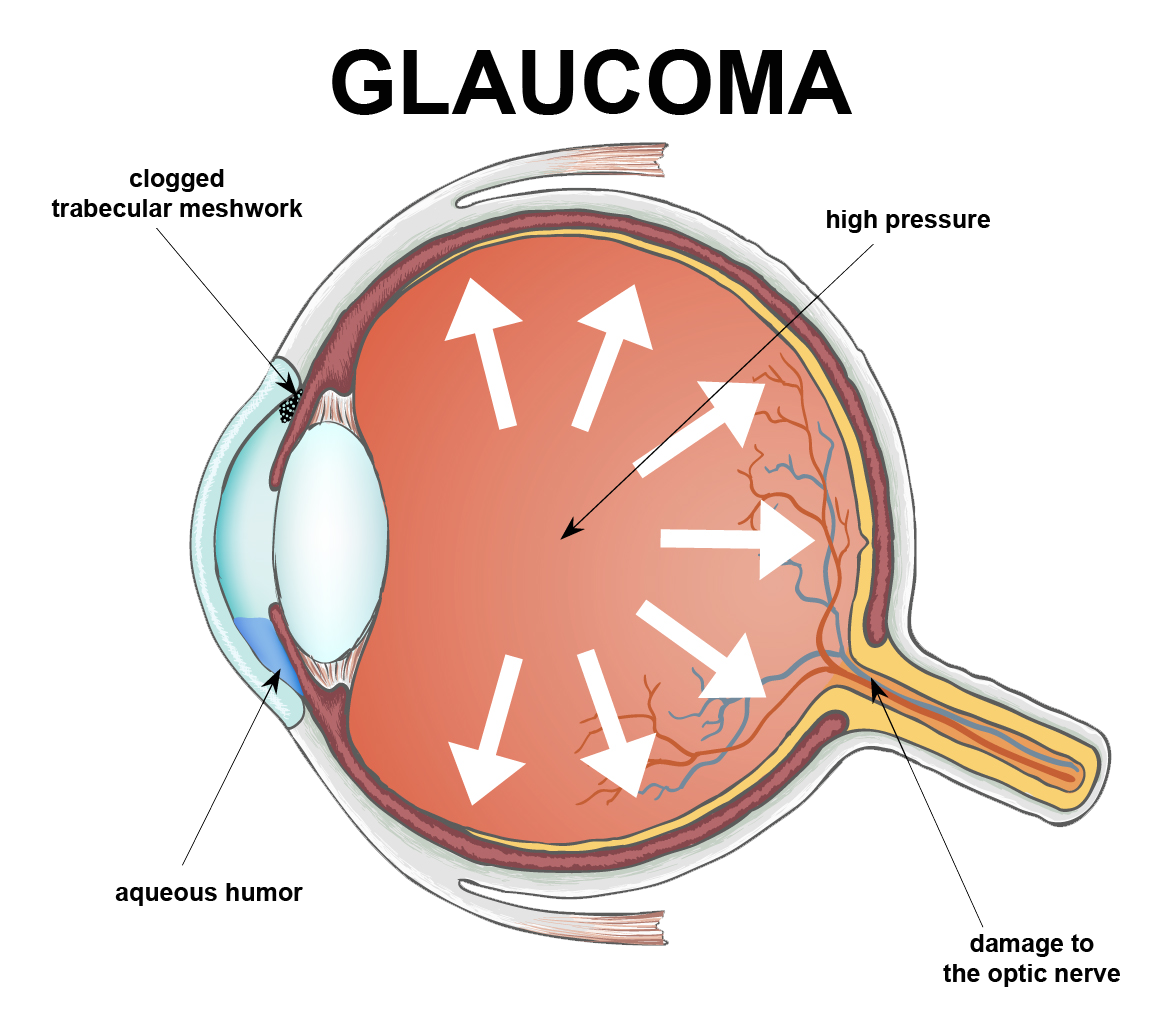
 National Glaucoma Awareness Month reminds all of us to get regular eye exams and show support for those suffering from this condition.
National Glaucoma Awareness Month reminds all of us to get regular eye exams and show support for those suffering from this condition.