Two hallmark DEF-funded projects are converging, providing great hope for those facing vision loss from retinitis pigmentosa (RP) or age-related macular degeneration (AMD).
The first project, headed by UC Irvine researchers Drs. Henry Klassen and Jing Yang, concentrates on putting human retinal progenitor cells into the eyes of those with RP in order to rescue damaged retinal cells. That project is currently in Phase II clinical trials, progressing toward FDA approval.
According to DEF Research Director Dr. Cristina Kenney, if the project is approved by the FDA for use with RP, the next question is: What other diseases might these retinal progenitor cells be used for? That’s where a second DEF-funded project comes in.
Kenney is working on a “personalized” cybrid cell model to screen agents that specifically target the mitochondria in AMD cells. To date, the researchers have different cybrid cell lines representing 60 different individuals with eye diseases. They are looking for novel mechanisms to protect AMD cells from dying.
Yang and Kenney are now working together to determine whether the retinal progenitor cells can be the agent that rescues AMD cybrids. “When we take the mitochondria from AMD patients and put them into healthy retinal cells, which makes cybrids, we have shown that these AMD cybrid cells will start to die. So we used that model to ask the question: How do we rescue them?” Kenney says.
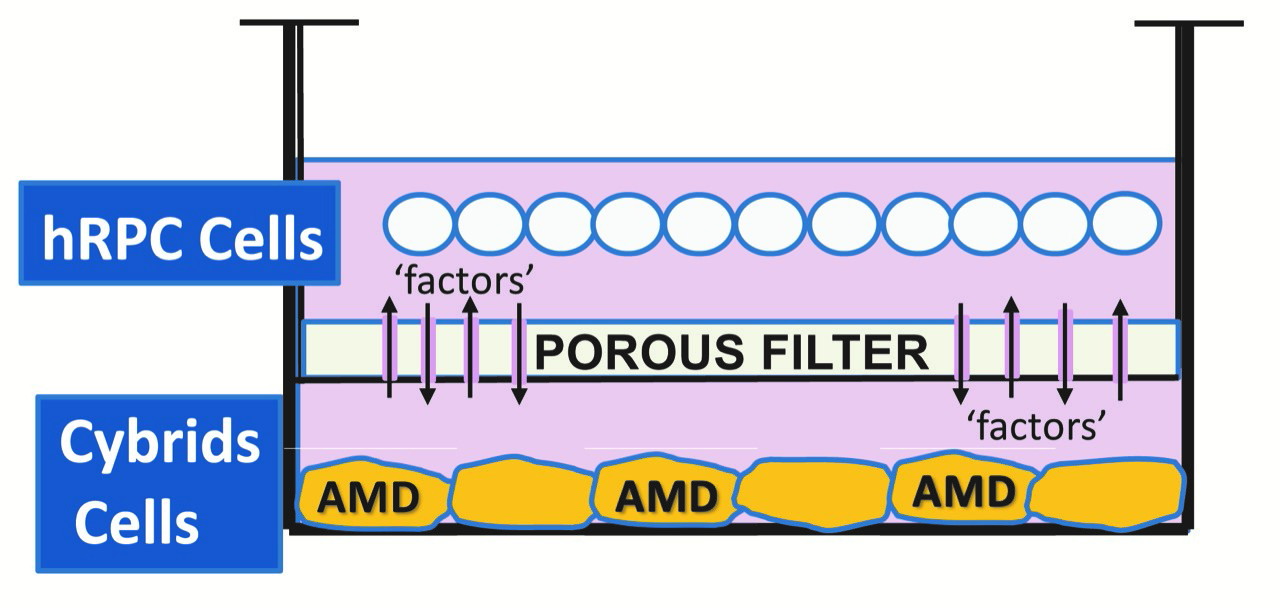
Kenney and Yang developed a tissue culture model, where the retinal progenitor cells are grown in one part of a chamber, and the AMD cybrids are grown in another part of chamber, surrounded by culture medium. There is a porous separator between the two chambers through which the cells can communicate.
“We are finding that the retinal progenitor cells produce a factor that protects the AMD cybrids,” Kenney says. “This provides promising evidence that these proprietary retinal progenitor cells that are being tested for treating RP also may be helpful in AMD patients.”
“DEF has been supporting both these retina-related projects for quite some time, and it’s very exciting to see them coming together to potentially treat both RP and AMD.”





 The past year has taken a toll on the physical and mental health of millions of people. While we were rightly focused on slowing the spread of the pandemic, widespread shutdowns brought about a more sedentary, inactive lifestyle, which has led to increased weight gain and worsened mental health for many. As we look ahead and as more people receive the vaccine, it is time to start reprioritizing physical activity and placing much needed attention on our health.
The past year has taken a toll on the physical and mental health of millions of people. While we were rightly focused on slowing the spread of the pandemic, widespread shutdowns brought about a more sedentary, inactive lifestyle, which has led to increased weight gain and worsened mental health for many. As we look ahead and as more people receive the vaccine, it is time to start reprioritizing physical activity and placing much needed attention on our health.




 Rest and blink your eyes – Researchers found that over 30% of people using digital devices rarely take time to rest their eyes. Just over 10% say they never take a break, even when working from home. The eye muscles get overworked and don’t get a chance to relax and recover. Experts suggest the 20-20-20 rule; every 20 minutes, focus your eyes and attention on something 20 feet away for 20 seconds. You can also get up and walk around for a few minutes.
Rest and blink your eyes – Researchers found that over 30% of people using digital devices rarely take time to rest their eyes. Just over 10% say they never take a break, even when working from home. The eye muscles get overworked and don’t get a chance to relax and recover. Experts suggest the 20-20-20 rule; every 20 minutes, focus your eyes and attention on something 20 feet away for 20 seconds. You can also get up and walk around for a few minutes. Reduce exposure to blue light – In the spectrum of light, blue is more high energy and close to ultraviolet light. So, if you use screens throughout the day, ask your eye doctor about the value of computer glasses that block blue light. Reducing exposure to blue light may help lessen vision problems. At home, using digital devices until bedtime can overstimulate your brain and make it more difficult to fall asleep. Eye doctors recommend no screen time at least one to two hours before going to sleep.
Reduce exposure to blue light – In the spectrum of light, blue is more high energy and close to ultraviolet light. So, if you use screens throughout the day, ask your eye doctor about the value of computer glasses that block blue light. Reducing exposure to blue light may help lessen vision problems. At home, using digital devices until bedtime can overstimulate your brain and make it more difficult to fall asleep. Eye doctors recommend no screen time at least one to two hours before going to sleep. Sit up straight – Proper posture is important. Your back should be straight and your feet on the floor while you work. Elevate your wrists slightly instead of resting them on the keyboard.
Sit up straight – Proper posture is important. Your back should be straight and your feet on the floor while you work. Elevate your wrists slightly instead of resting them on the keyboard. Set up monitor properly – Make sure your computer screen is about 25 inches, or an arm’s length, away from your face. The center of the screen should be about 10-15 degrees below eye level. Cut glare by using a matte screen filter. You can find them for all types of computers, phones, and tablets. Increase font size or set the magnification of the documents you are reading to a comfortable size.
Set up monitor properly – Make sure your computer screen is about 25 inches, or an arm’s length, away from your face. The center of the screen should be about 10-15 degrees below eye level. Cut glare by using a matte screen filter. You can find them for all types of computers, phones, and tablets. Increase font size or set the magnification of the documents you are reading to a comfortable size. Consider computer glasses –For the greatest comfort at your computer, you might benefit from having your eye doctor modify your eyeglasses prescription to create customized computer glasses. This is especially true if you normally wear distance contact lenses, which may also become dry and uncomfortable during extended screen time. Computer glasses also are a good choice if you wear bifocals or progressive lenses, because these lenses generally are not optimal for the distance to your computer screen.
Consider computer glasses –For the greatest comfort at your computer, you might benefit from having your eye doctor modify your eyeglasses prescription to create customized computer glasses. This is especially true if you normally wear distance contact lenses, which may also become dry and uncomfortable during extended screen time. Computer glasses also are a good choice if you wear bifocals or progressive lenses, because these lenses generally are not optimal for the distance to your computer screen. Get an Eye Exam – If you have tried all these tips and eye strain is still an issue, it might be time to see an eye care professional to schedule an eye exam. The exam may even detect underlying issues before they becomes worse.
Get an Eye Exam – If you have tried all these tips and eye strain is still an issue, it might be time to see an eye care professional to schedule an eye exam. The exam may even detect underlying issues before they becomes worse.
 Taking care of your health is critical and you may have concerns related to eye health as a result of the COVID-19 pandemic. The offices of Ophthalmologists and Optometrists are resuming the delivery of comprehensive eye and vision care and implementing new protocols to provide care in a safe and healthy environment.
Taking care of your health is critical and you may have concerns related to eye health as a result of the COVID-19 pandemic. The offices of Ophthalmologists and Optometrists are resuming the delivery of comprehensive eye and vision care and implementing new protocols to provide care in a safe and healthy environment.

 Tom Sullivan
Tom Sullivan