Previously Approved Drug Shows Promise for Dry Age-Related Macular Degeneration (AMD)
Getting FDA approval for new treatments can take years or even decades. But what about repurposing drugs that have already been approved for other diseases? That’s precisely the question DEF-supported researchers are asking about a new treatment for dry age-related macular degeneration (AMD) and other aging diseases, including Alzheimer’s and Parkinson’s.
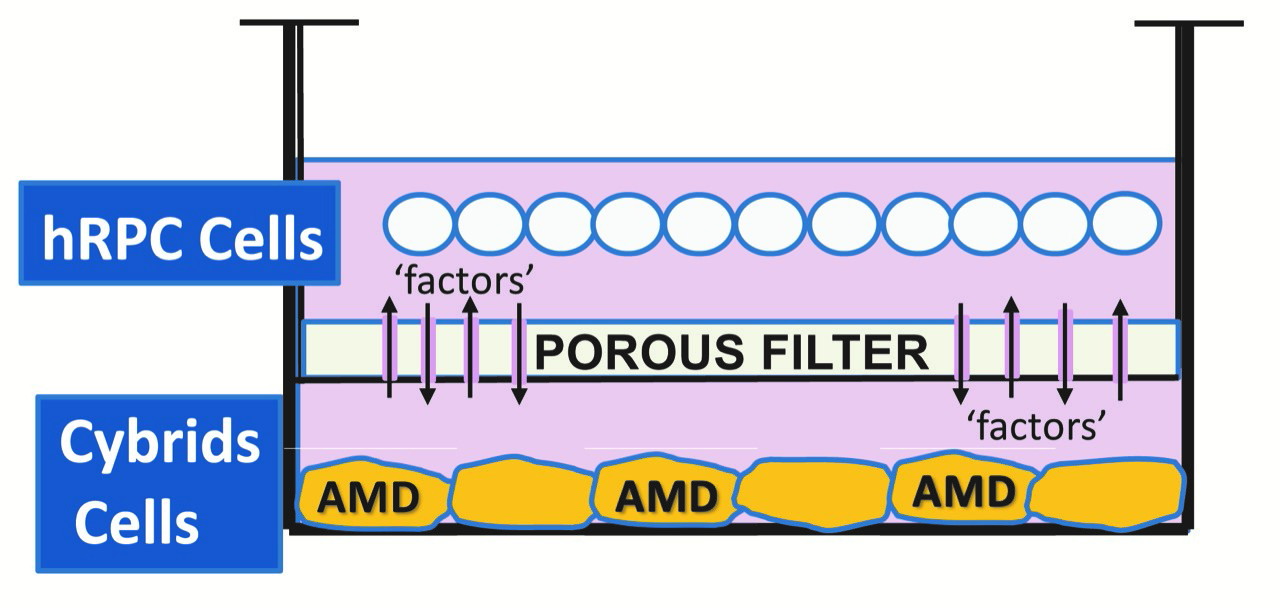
Six years ago, DEF Research Director Dr. Cristina Kenney began collaborating with Parkinson’s specialist Dr. Howard Federoff of the Department of Neurology at UC Irvine. DEF-supported researchers had previously shown that damaged mitochondria are a significant factor in accelerating cell death in AMD, and Kenney developed a cybrid mitochondria model to study AMD. Federoff had set up a screening system to look at drugs previously approved by the FDA that might improve the health of mitochondria, whose demise also contribute to Parkinson’s and Alzheimer’s. Of more than a thousand drugs screened, he identified 13 that could rejuvenate mitochondria. Kenney’s cell-culture models and Federoff’s system were a match made in research heaven.
Together, the researchers homed in on one drug, which Federoff named PU-91, because it was the 91st drug he’d tested. “When we added PU-91 to our AMD cybrids, the cells lived longer, they functioned better the damage to the mitochondria was decreased and it really improved the health of the mitochondria,” Kenney says. “PU-91 is a drug called fenofibrate, which has been used for years to treat high cholesterol. When this drug is modified slightly, it helps sluggish mitochondria regain their health. We’re taking a drug that has been used for many years with FDA approval, and we’re repurposing it for a new target and new types of diseases.”
Benefits of Repurposing
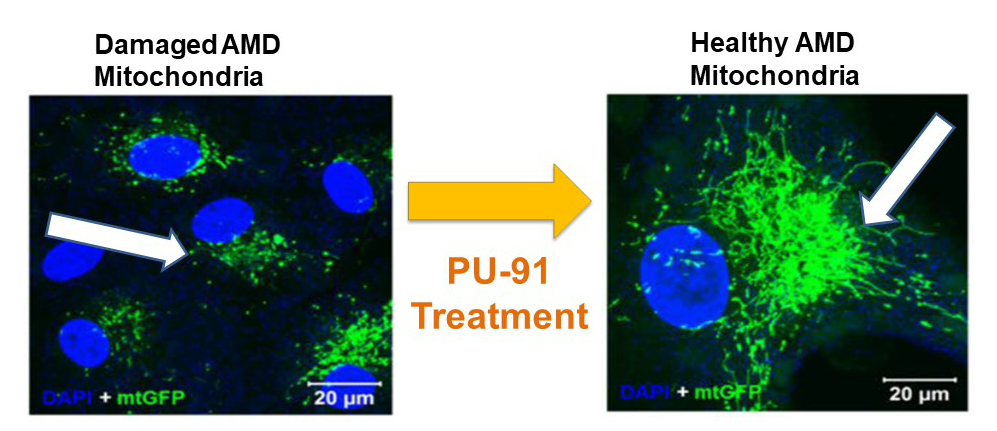
Tremendous savings of time and money are to be had by repurposing a known drug rather than starting with a drug people have never used before. Perhaps most importantly, because it’s been used for so many years in patients, the known drug has a proven safety track record. PU-91 has an additional advantage in that it is taken orally. While there is currently one type of treatment for wet AMD — an injection — there is no treatment at all for the dry form of AMD. An oral treatment for dry AMD is a game-changer.
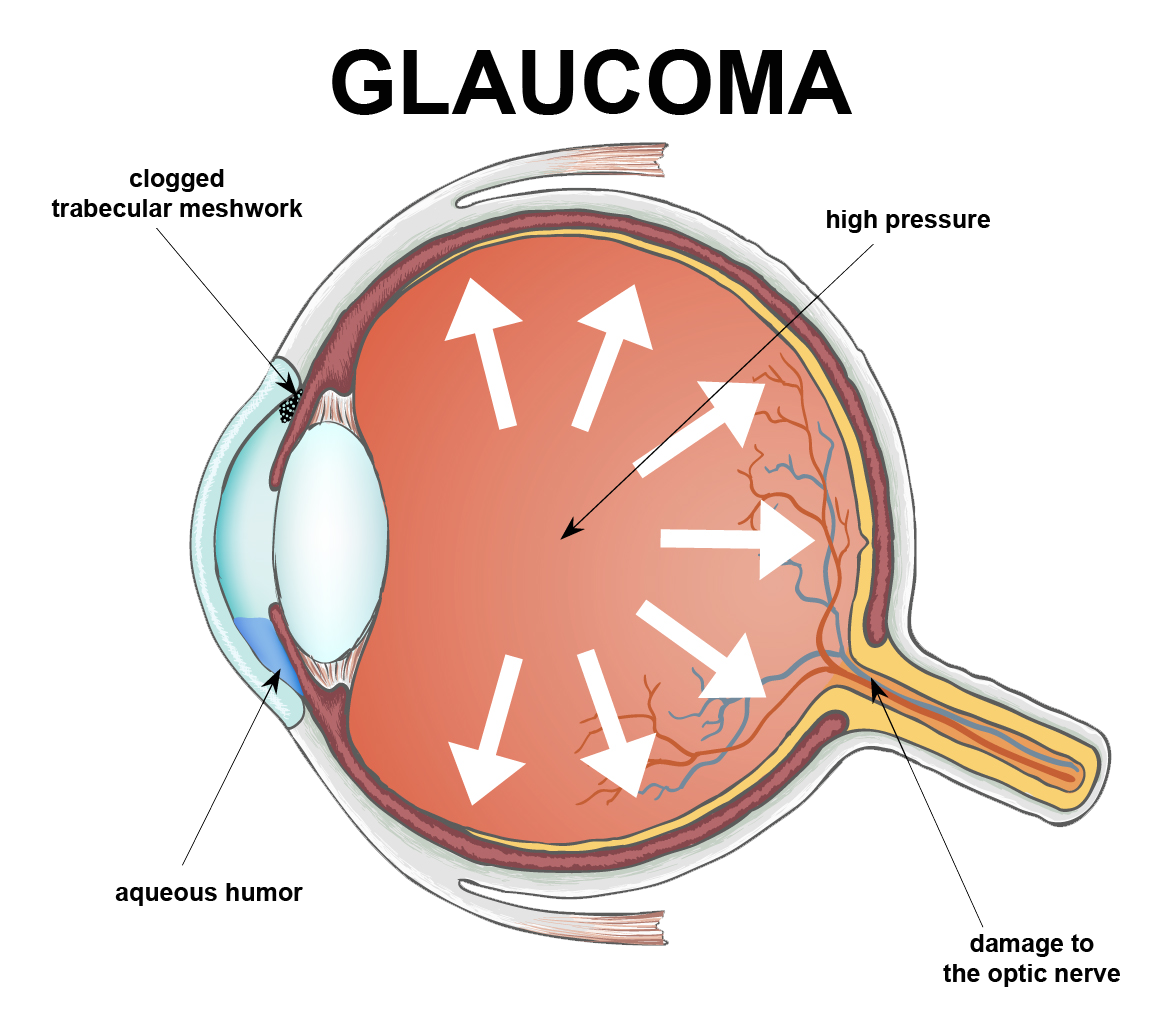
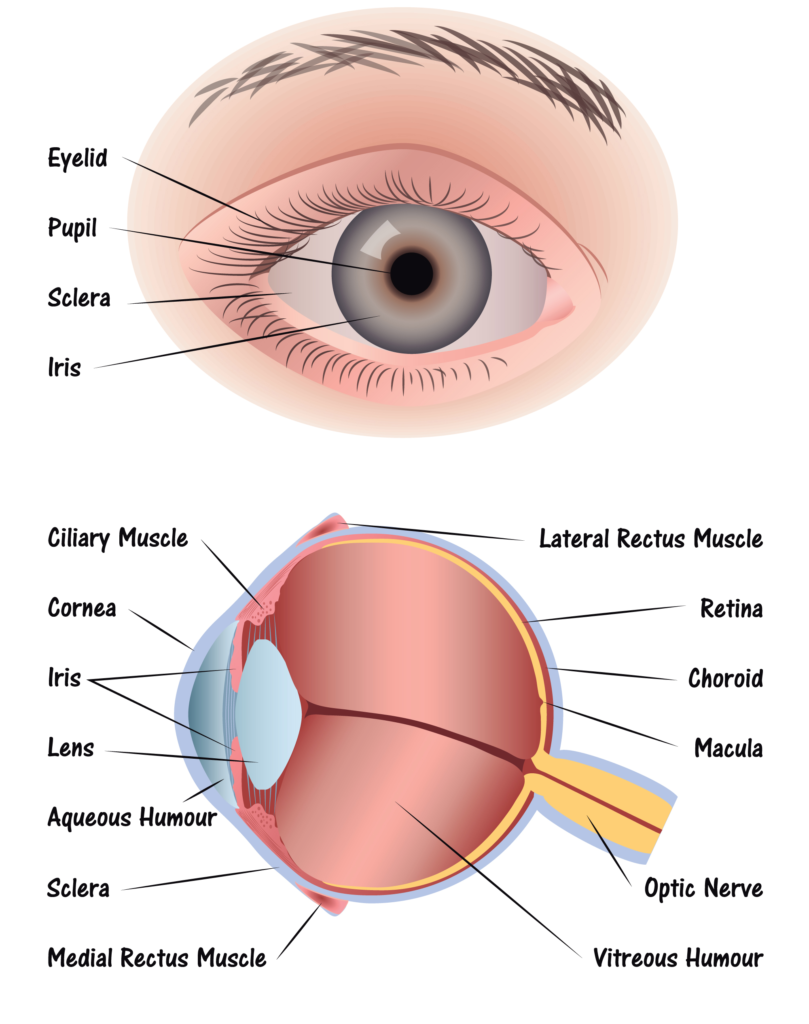
The research is going so well that a company has been formed specifically to bring this drug to market for dry AMD. “As we become more successful, this type of drug can also be used for neurodegenerative diseases that have damaged mitochondria, such as Parkinson’s disease and Alzheimer’s disease,” Kenney says. “Potentially, it might even be used for something, such as glaucoma, that causes cell death of the retina ganglion cells in the eye. There are a lot of potential uses for it.”
Bench to Bedside
DEF currently is supporting ongoing studies to optimize PU-91’s formulations for maximum effectiveness in patients with AMD. “It’s exciting, because this is the goal for translational researchers,” Kenney says. “Take what you’re doing at the bench and bring it to the bedside.”


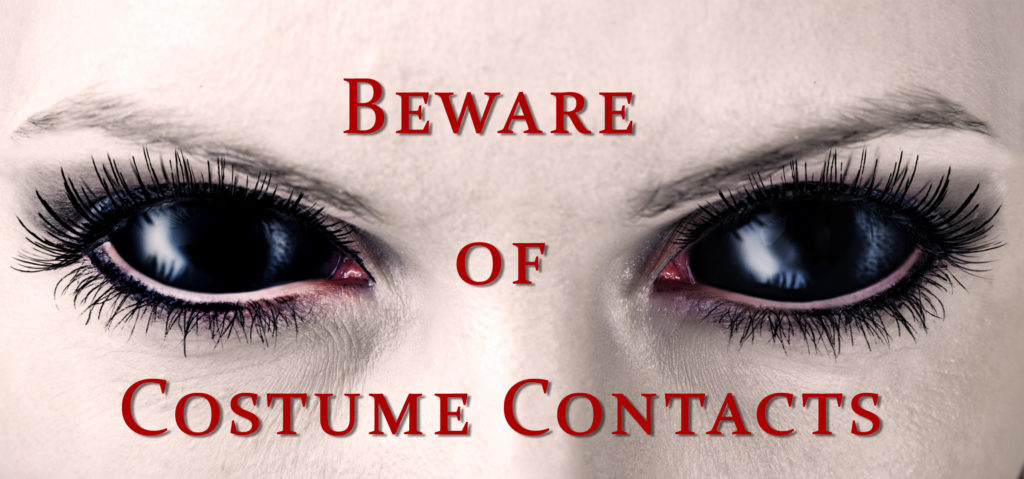 Costume Contact Lenses such as cat eyes or zombie may make your Halloween costume a bit more frightful although wearing those lenses without a prescription can be more terrifying, as it could result in vision loss or even blindness.
Costume Contact Lenses such as cat eyes or zombie may make your Halloween costume a bit more frightful although wearing those lenses without a prescription can be more terrifying, as it could result in vision loss or even blindness.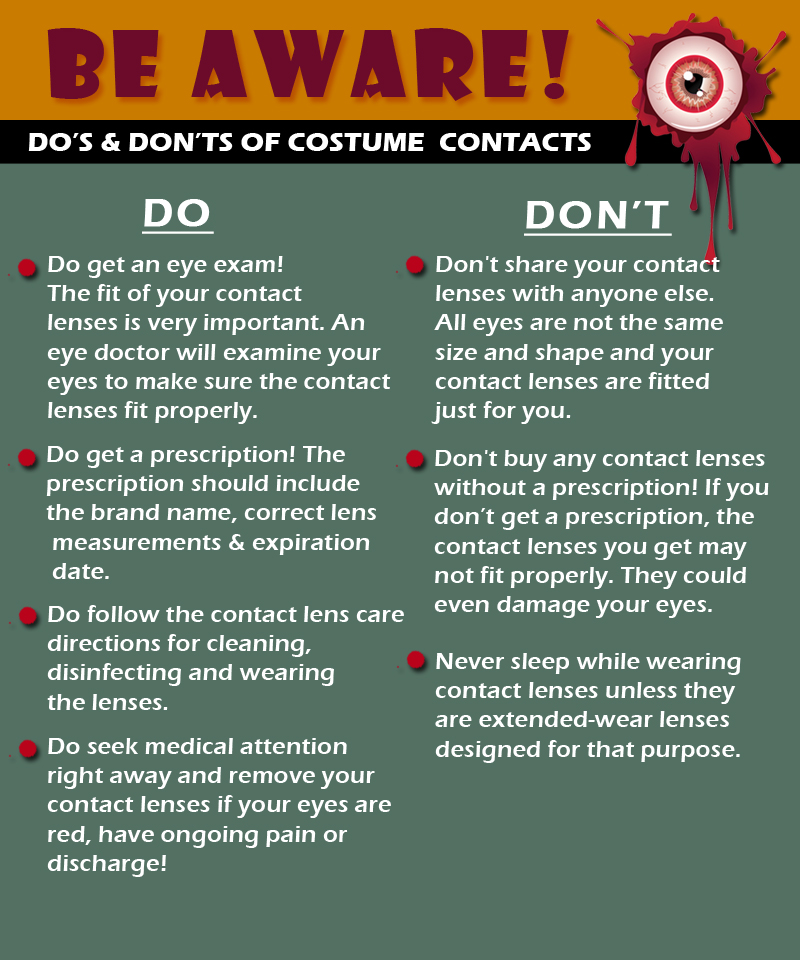










 Rest and blink your eyes – Researchers found that over 30% of people using digital devices rarely take time to rest their eyes. Just over 10% say they never take a break, even when working from home. The eye muscles get overworked and don’t get a chance to relax and recover. Experts suggest the 20-20-20 rule; every 20 minutes, focus your eyes and attention on something 20 feet away for 20 seconds. You can also get up and walk around for a few minutes.
Rest and blink your eyes – Researchers found that over 30% of people using digital devices rarely take time to rest their eyes. Just over 10% say they never take a break, even when working from home. The eye muscles get overworked and don’t get a chance to relax and recover. Experts suggest the 20-20-20 rule; every 20 minutes, focus your eyes and attention on something 20 feet away for 20 seconds. You can also get up and walk around for a few minutes. Reduce exposure to blue light – In the spectrum of light, blue is more high energy and close to ultraviolet light. So, if you use screens throughout the day, ask your eye doctor about the value of computer glasses that block blue light. Reducing exposure to blue light may help lessen vision problems. At home, using digital devices until bedtime can overstimulate your brain and make it more difficult to fall asleep. Eye doctors recommend no screen time at least one to two hours before going to sleep.
Reduce exposure to blue light – In the spectrum of light, blue is more high energy and close to ultraviolet light. So, if you use screens throughout the day, ask your eye doctor about the value of computer glasses that block blue light. Reducing exposure to blue light may help lessen vision problems. At home, using digital devices until bedtime can overstimulate your brain and make it more difficult to fall asleep. Eye doctors recommend no screen time at least one to two hours before going to sleep. Sit up straight – Proper posture is important. Your back should be straight and your feet on the floor while you work. Elevate your wrists slightly instead of resting them on the keyboard.
Sit up straight – Proper posture is important. Your back should be straight and your feet on the floor while you work. Elevate your wrists slightly instead of resting them on the keyboard. Set up monitor properly – Make sure your computer screen is about 25 inches, or an arm’s length, away from your face. The center of the screen should be about 10-15 degrees below eye level. Cut glare by using a matte screen filter. You can find them for all types of computers, phones, and tablets. Increase font size or set the magnification of the documents you are reading to a comfortable size.
Set up monitor properly – Make sure your computer screen is about 25 inches, or an arm’s length, away from your face. The center of the screen should be about 10-15 degrees below eye level. Cut glare by using a matte screen filter. You can find them for all types of computers, phones, and tablets. Increase font size or set the magnification of the documents you are reading to a comfortable size. Consider computer glasses –For the greatest comfort at your computer, you might benefit from having your eye doctor modify your eyeglasses prescription to create customized computer glasses. This is especially true if you normally wear distance contact lenses, which may also become dry and uncomfortable during extended screen time. Computer glasses also are a good choice if you wear bifocals or progressive lenses, because these lenses generally are not optimal for the distance to your computer screen.
Consider computer glasses –For the greatest comfort at your computer, you might benefit from having your eye doctor modify your eyeglasses prescription to create customized computer glasses. This is especially true if you normally wear distance contact lenses, which may also become dry and uncomfortable during extended screen time. Computer glasses also are a good choice if you wear bifocals or progressive lenses, because these lenses generally are not optimal for the distance to your computer screen. Get an Eye Exam – If you have tried all these tips and eye strain is still an issue, it might be time to see an eye care professional to schedule an eye exam. The exam may even detect underlying issues before they becomes worse.
Get an Eye Exam – If you have tried all these tips and eye strain is still an issue, it might be time to see an eye care professional to schedule an eye exam. The exam may even detect underlying issues before they becomes worse.
 Step 1: Light passes through a thin layer of moisture
Step 1: Light passes through a thin layer of moisture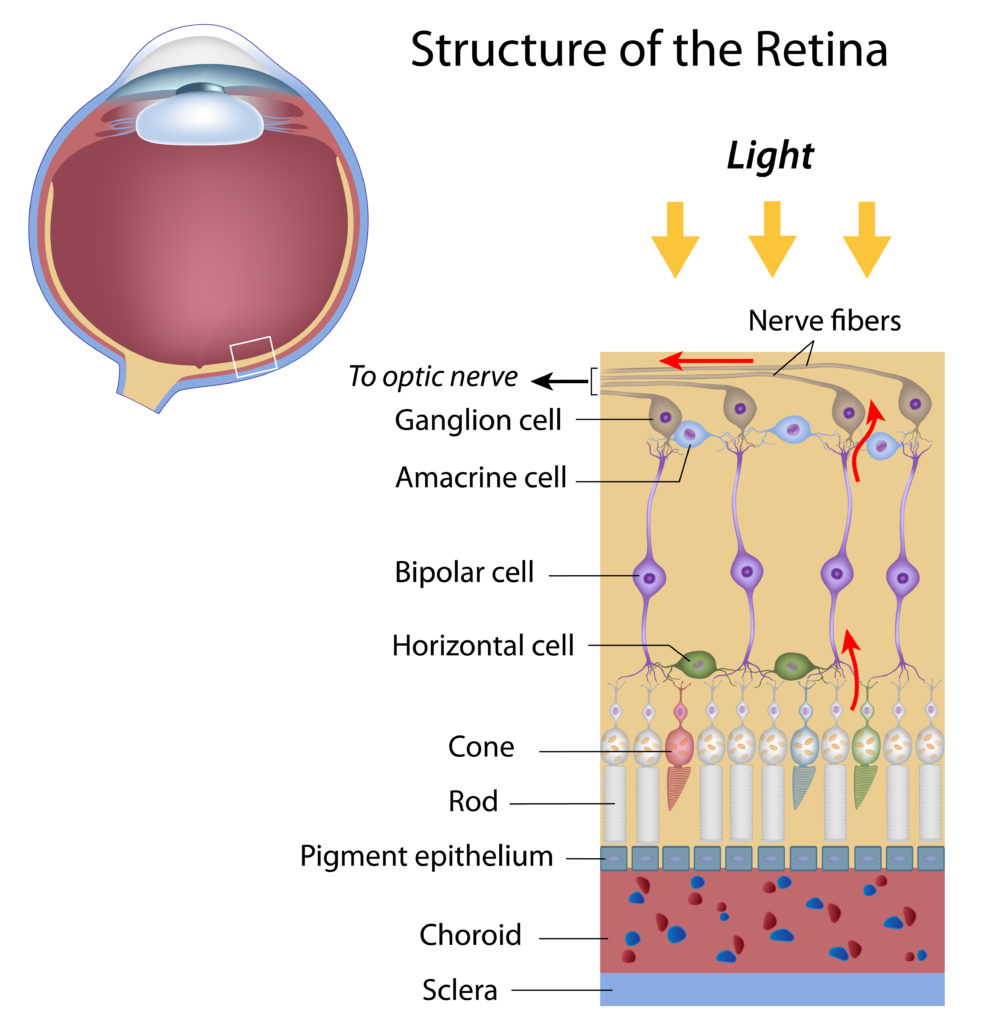
 National Glaucoma Awareness Month reminds all of us to get regular eye exams and show support for those suffering from this condition.
National Glaucoma Awareness Month reminds all of us to get regular eye exams and show support for those suffering from this condition.