 Healthy Aging Month is an annual health observance designed to focus national attention on the positive aspects of growing older. Aging is a process that brings many changes. Vision loss and blindness, however, do not have to be one of them. There are several simple steps you can take to help keep your eyes healthy for the rest of your life.
Healthy Aging Month is an annual health observance designed to focus national attention on the positive aspects of growing older. Aging is a process that brings many changes. Vision loss and blindness, however, do not have to be one of them. There are several simple steps you can take to help keep your eyes healthy for the rest of your life.
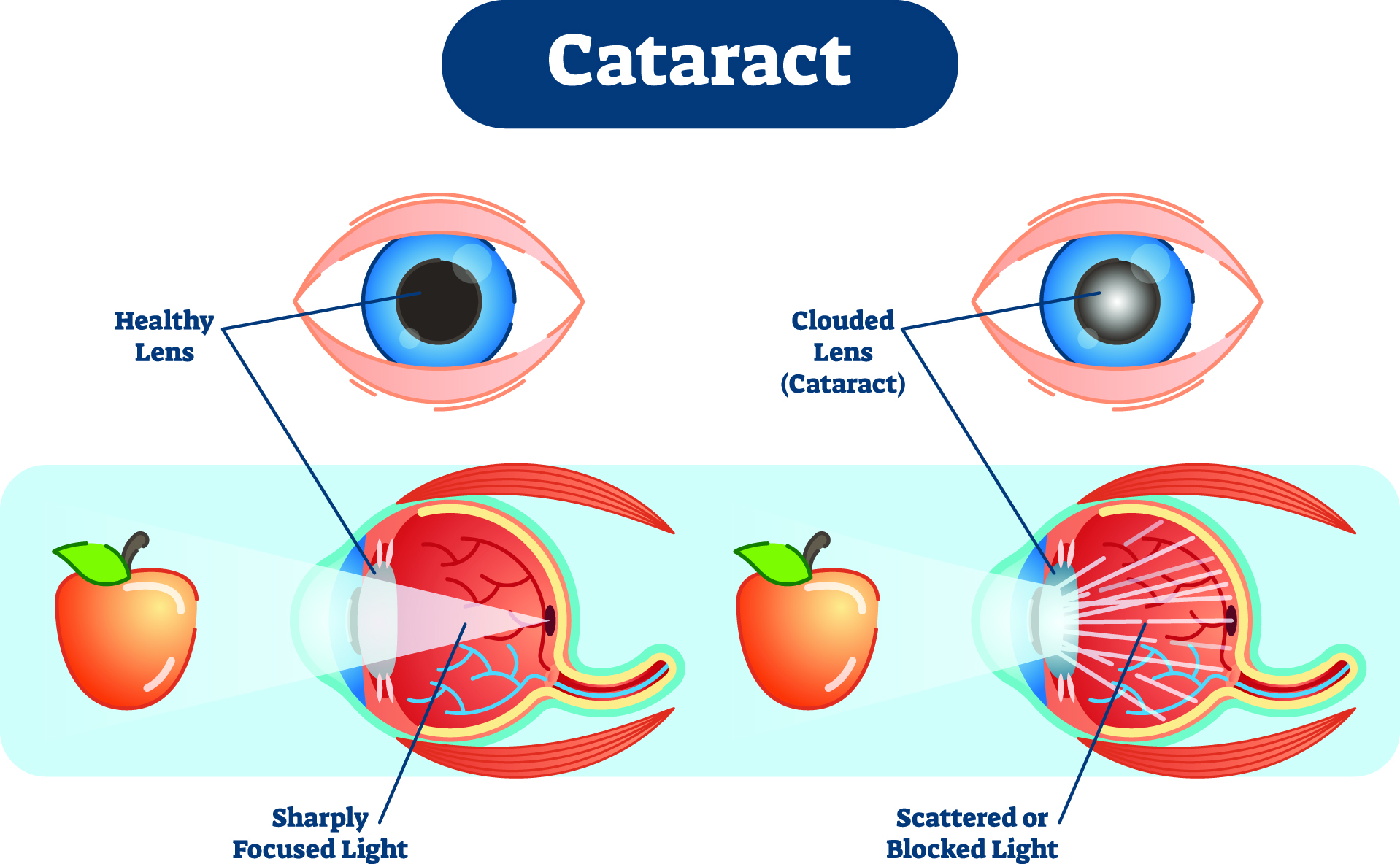
Eye diseases often have no early symptoms, but can be detected during a comprehensive dilated eye exam. A comprehensive dilated eye exam is different from the basic eye exam or screening you have for glasses or contacts. By dilating the pupils and examining the back of the eyes, your eye care professional can detect eye diseases in their early stages, before vision loss occurs. By performing a comprehensive eye exam, your eye care professional can check for early signs of –
Here are some other tips to maintain healthy vision now and as you age:

- Eat a healthy, balanced diet. Fruits and vegetables can help keep your eyes healthy. Visit our website for healthy eye recipes, click here Eye Cook.
 Maintain a healthy weight. Being overweight increases your risk for diabetes. By exercising regularly, you can help keep your body healthy and prevent vision loss.
Maintain a healthy weight. Being overweight increases your risk for diabetes. By exercising regularly, you can help keep your body healthy and prevent vision loss.
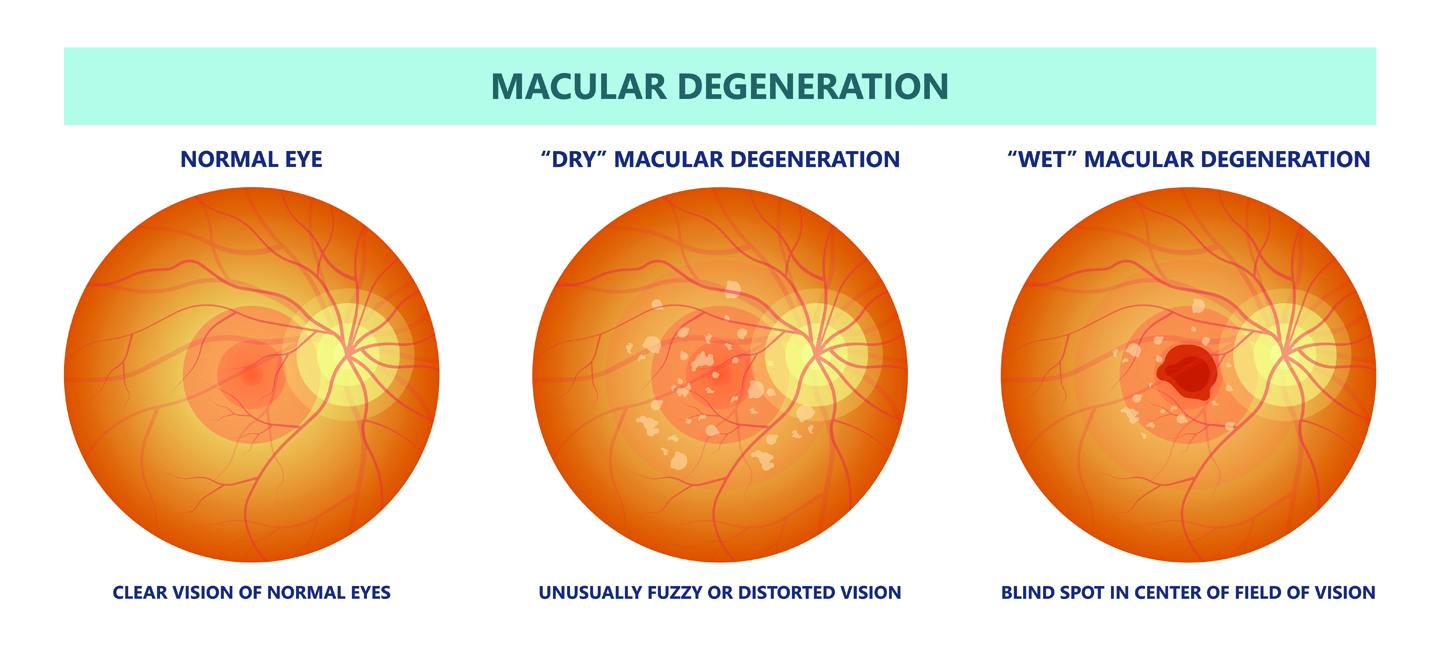
 Don’t smoke. Smoking increases your risk for age-related macular degeneration, cataract, and other eye diseases and conditions that can damage the optic nerve.
Don’t smoke. Smoking increases your risk for age-related macular degeneration, cataract, and other eye diseases and conditions that can damage the optic nerve.
 Wear protective eyewear when outdoors. Protecting your eyes from the sun’s ultraviolet rays when you are outdoors is vital for your eye health. Wearing sunglasses that block 99 to 100 percent of both UV-A and UV-B radiation.
Wear protective eyewear when outdoors. Protecting your eyes from the sun’s ultraviolet rays when you are outdoors is vital for your eye health. Wearing sunglasses that block 99 to 100 percent of both UV-A and UV-B radiation.
 Know your family history. Talk to your family members about their eye health history. It’s important to know if anyone has been diagnosed with a disease or condition since many are hereditary, such as glaucoma, macular degeneration, and diabetes . This will help determine if you are at higher risk for developing an eye disease or condition.
Know your family history. Talk to your family members about their eye health history. It’s important to know if anyone has been diagnosed with a disease or condition since many are hereditary, such as glaucoma, macular degeneration, and diabetes . This will help determine if you are at higher risk for developing an eye disease or condition.
 Consider a multivitamin. Vitamins C, E and the mineral zinc have been shown to promote eye health. Vitamins with Lutein and Zeaxanthin have been known to help patients with moderate to severe age-related macular degeneration.
Consider a multivitamin. Vitamins C, E and the mineral zinc have been shown to promote eye health. Vitamins with Lutein and Zeaxanthin have been known to help patients with moderate to severe age-related macular degeneration.
 Give your eyes a rest. If you spend a lot of time at the computer or focusing at any one distance, you sometimes forget to blink, resulting in dryness and eye fatigue. Every 20 minutes, look away about 20 feet in front of you for 20 seconds. This can help reduce eyestrain. Consider using a lubricant eye drop during long periods of intense eye use and rest your eyes for 5 minutes.
Give your eyes a rest. If you spend a lot of time at the computer or focusing at any one distance, you sometimes forget to blink, resulting in dryness and eye fatigue. Every 20 minutes, look away about 20 feet in front of you for 20 seconds. This can help reduce eyestrain. Consider using a lubricant eye drop during long periods of intense eye use and rest your eyes for 5 minutes.
You can’t stop time, but you can take care of your eyes so that they remain healthy as you age. Having a healthy vision can be possible at any age! Even if you are not experiencing vision problems, visiting an eye care professional regularly for a comprehensive dilated eye exam is the most important thing you can do to reduce your risk of vision loss as you age.
Download “Everyone’s vision can change with age”
A handout with explanation on how vision can change with age.



 Thank You to all who helped support DEF
Thank You to all who helped support DEF  In the house: When using household chemicals, read the instructions and labels carefully, work in a well-ventilated area and make sure to point spray nozzles away from you. Many chemicals are extremely hazardous and can permanently damage the surface of your eyes, resulting in some loss of vision or even blindness.
In the house: When using household chemicals, read the instructions and labels carefully, work in a well-ventilated area and make sure to point spray nozzles away from you. Many chemicals are extremely hazardous and can permanently damage the surface of your eyes, resulting in some loss of vision or even blindness. In the garage/workshop: Wear protective eyewear to shield your eyes from flying fragments, fumes, dust particles, sparks and splashing chemicals. Power tools can also send wood chips or other substances flying into the air. Many objects can fly into your eyes unexpectedly and cause injury.
In the garage/workshop: Wear protective eyewear to shield your eyes from flying fragments, fumes, dust particles, sparks and splashing chemicals. Power tools can also send wood chips or other substances flying into the air. Many objects can fly into your eyes unexpectedly and cause injury. In the yard/garden: Put on protective eyewear before you use a lawnmower, power trimmer or edger and be sure to check for rocks and stones because they can become dangerous projectiles as they shoot from these machines.
In the yard/garden: Put on protective eyewear before you use a lawnmower, power trimmer or edger and be sure to check for rocks and stones because they can become dangerous projectiles as they shoot from these machines.
 Make sure they take frequent screen breaks. Instead of focusing directly on the screen, encourage your child to look around the room every now and then, or take some time to stare out the window (at least 20 seconds is recommended by the American Optometric Association). You can even remind them to blink.
Make sure they take frequent screen breaks. Instead of focusing directly on the screen, encourage your child to look around the room every now and then, or take some time to stare out the window (at least 20 seconds is recommended by the American Optometric Association). You can even remind them to blink. It’s easy for us to forget about our eyes let alone our child’s, but it is very important to get your child’s eyes checked regularly.
It’s easy for us to forget about our eyes let alone our child’s, but it is very important to get your child’s eyes checked regularly. As winter shifts to spring, and flowers, grasses and trees begin to bloom, spring can take a toll on your eyes if you suffer from seasonal allergies. The spring season has a marked an increase in pollen and allergens in the air, that leave you with congestion, headaches, and itchy, swollen eyes, known as eye allergies.
As winter shifts to spring, and flowers, grasses and trees begin to bloom, spring can take a toll on your eyes if you suffer from seasonal allergies. The spring season has a marked an increase in pollen and allergens in the air, that leave you with congestion, headaches, and itchy, swollen eyes, known as eye allergies.