Children and their phones, iPads and gaming devices are inseparable today. Most are growing up with a wide selection of electronic devices at their fingertips. They can’t imagine a world without the internet, smartphones and tablets. Although, all that reading and playing games on their handheld devices may be harmful. But it’s not just kids who are getting too much screen time. Many parents struggle with over use of screen time themselves. So it’s important to understand how too much screen time could be harming everyone in the family.
 Children can experience at least one of the following symptoms after being exposed to more than two hours of screen time per day:
Children can experience at least one of the following symptoms after being exposed to more than two hours of screen time per day:
- Headaches
- Neck/shoulder pain
- Eye strain, dry or irritated eyes
- Reduced attention span
- Poor behavior
- Irritability
Any of these symptoms could potentially affect academic performance and social interactions.
The worldwide rapid rise of nearsightedness has been linked to increased use of and exposure to electronic devices. However, spending more time outdoors, especially in early childhood, can decrease the progression of nearsightedness.
Blue Light can be harmful
 The LED screens of computers and portable digital devices emit a broad spectrum of visible light. Most of these light rays are harmless, but a portion of the light emitted by these screens is relatively high-energy visible light called “blue light.”
The LED screens of computers and portable digital devices emit a broad spectrum of visible light. Most of these light rays are harmless, but a portion of the light emitted by these screens is relatively high-energy visible light called “blue light.”
Blue light has shorter wavelengths and higher energy than other visible light rays. Some laboratory research suggests certain bands of blue light may be harmful to the light-sensitive retina of the eye over time.
Blue light also plays an important role in regulating our body’s circadian rhythm. This basically is an internal clock that’s running in our brain and cycles between alertness and sleepiness at regular intervals over a 24-hour period.
Too much exposure to blue light at the wrong time of day can disrupt a person’s normal sleep/wake cycle, which can have serious health consequences. Sleep disruption can be especially problematic for children, leading to daytime drowsiness and poor performance in school. Some authorities feel that disruption of the sleep/wake cycle also can eventually lead to weight gain and obesity-related health problems.
Research has shown that people who experience disrupted 24-hour cycles of sleep and activity also are more likely to have mood disorders, lower levels of happiness and greater feelings of loneliness.
How to cut back on screen time
- Set a limit on daily screen time. Make it clear to your kids and stick to it.
- Encourage your child to spend some of that screen-free time outdoors while it is still light.
- Establish screen-free zones: For example, no smartphone use for anyone in the family in the car, at restaurants, or at the dinner table.
- No screens in the bedroom when it is time for bed. No exceptions.
- As parents you can be a model for moderate screen use. Show your children, with your own behavior, how to live a rich, varied and healthy life where all habits are practiced in moderation.
It is also very important to teach your child good eye habits, below are few tips from experts:
- You can set a kitchen timer or a smart device timer to remind them.
- Alternate reading an e-book with a real book and encourage kids to look up and out the window every two chapters.
- After completing a level in a video game, look out the window for 20 seconds.
- Pre-mark books with a paperclip every few chapters to remind your child to look up. On an e-book, use the “bookmark” function for the same effect.
- Avoid using a computer outside or in brightly lit areas, as the glare on the screen can create eye strain.
- Adjust the brightness and contrast of your computer screen so that it feels comfortable to you.
- Use good posture when using a computer and when reading.
- Encourage your child to hold digital media farther away, 18 to 24 inches is ideal.
- Create a distraction that causes your child to look up every now and then.
- Remind them to blink when watching a screen.
Finally, it is very important to make sure your child gets a regular eye exam by a pediatric ophthalmologist or optometrist. This will help monitor your child’s vision and eye health.


 Tom Sullivan
Tom Sullivan

 Lauren Hauptman
Lauren Hauptman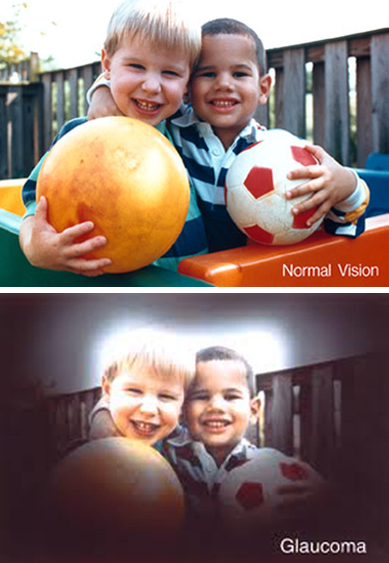
 The other day my daughter Blythe asked me which Christmas I consider to be my favorite. I had to think a minute, because as a family, the Sullivan’s have had some great ones. I was about to say the first time you and your brother Tom were old enough to really get into Santa, being absolutely sure that the fat man brought your presents right down the chimney. I was about to say that, and then I remembered.
The other day my daughter Blythe asked me which Christmas I consider to be my favorite. I had to think a minute, because as a family, the Sullivan’s have had some great ones. I was about to say the first time you and your brother Tom were old enough to really get into Santa, being absolutely sure that the fat man brought your presents right down the chimney. I was about to say that, and then I remembered.  Colorado, when our children were teenagers and our friend, the marvelous Betty White, joined us for a Christmas Eve sleigh ride none of us will ever forget. The night was perfect. It had snowed earlier that day, and the air had a feeling of Christmas that you could almost taste. Oh, sure, it was cold, but we were bundled up under tons of blankets as two beautiful Clydesdale horses with bells jingling took us through the woods to a magical barn where dinner would be served and carols sung.
Colorado, when our children were teenagers and our friend, the marvelous Betty White, joined us for a Christmas Eve sleigh ride none of us will ever forget. The night was perfect. It had snowed earlier that day, and the air had a feeling of Christmas that you could almost taste. Oh, sure, it was cold, but we were bundled up under tons of blankets as two beautiful Clydesdale horses with bells jingling took us through the woods to a magical barn where dinner would be served and carols sung.  Tom Sullivan
Tom Sullivan Harsh weather conditions can reduce the natural moisture in your eyes and the irritation usually results in a burning or itching sensation that often leads to rubbing or scratching your eyes which can worsen the symptoms. Sometimes it feels like there is a foreign object in your eye and for some, dry eyes can even cause excessive tearing, as your eyes try to overcompensate for their lack of protective tears. Prolonged, untreated dry eyes can lead to blurred vision as well. Between the harsh winter winds outside and the dry heat radiating inside, our eyes are very quickly irritated and dried in the winter months. The result is itchy, dry eyes that may cause pain, blurred vision, a burning sensation, or even watery vision as our eyes try to compensate for the dryness.
Harsh weather conditions can reduce the natural moisture in your eyes and the irritation usually results in a burning or itching sensation that often leads to rubbing or scratching your eyes which can worsen the symptoms. Sometimes it feels like there is a foreign object in your eye and for some, dry eyes can even cause excessive tearing, as your eyes try to overcompensate for their lack of protective tears. Prolonged, untreated dry eyes can lead to blurred vision as well. Between the harsh winter winds outside and the dry heat radiating inside, our eyes are very quickly irritated and dried in the winter months. The result is itchy, dry eyes that may cause pain, blurred vision, a burning sensation, or even watery vision as our eyes try to compensate for the dryness. I can only imagine my wife’s beautiful face. Oh sure, I’ve touched it and kissed it many times. I’ve felt the lines with the tips of my fingers, tracing our lives together, and I’ve heard her smile. I understand that’s not really seeing it. It’s not seeing her eyes as they sparkle with something funny I said; or, when she looks at me with love reserved only for those who are truly in love.
I can only imagine my wife’s beautiful face. Oh sure, I’ve touched it and kissed it many times. I’ve felt the lines with the tips of my fingers, tracing our lives together, and I’ve heard her smile. I understand that’s not really seeing it. It’s not seeing her eyes as they sparkle with something funny I said; or, when she looks at me with love reserved only for those who are truly in love. Costume Contact Lenses such as cat eyes or zombie may make your Halloween costume a bit more frightful although wearing those lenses without a prescription can be more terrifying, as it could result in vision loss or even blindness.
Costume Contact Lenses such as cat eyes or zombie may make your Halloween costume a bit more frightful although wearing those lenses without a prescription can be more terrifying, as it could result in vision loss or even blindness.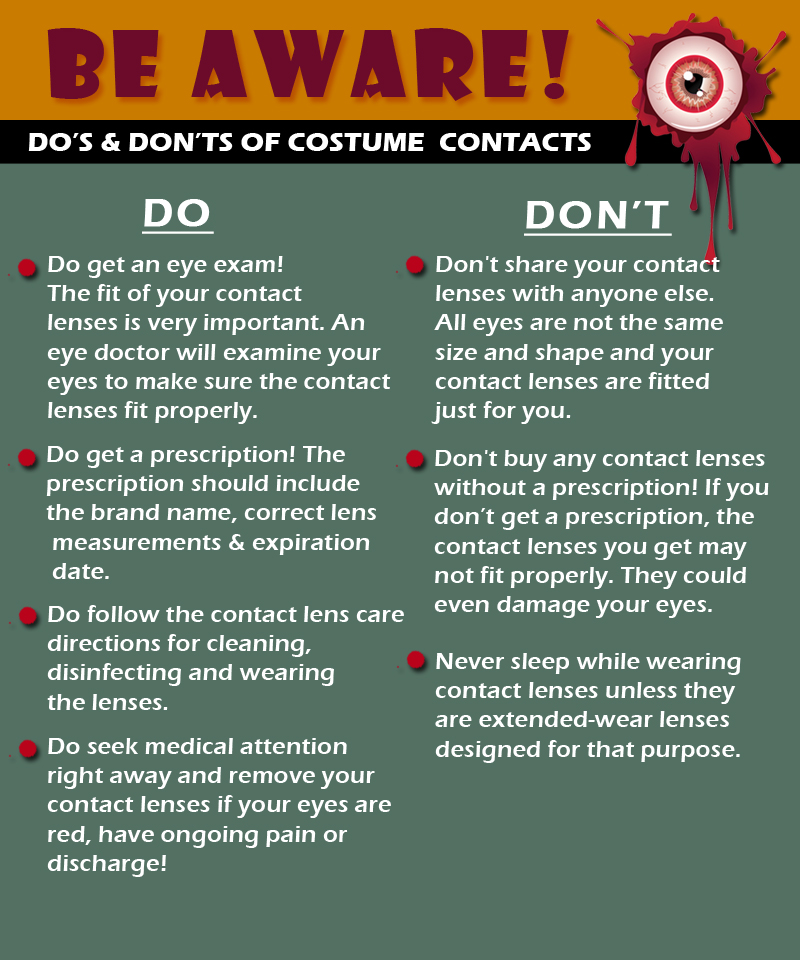
 I could hear Charlie rubbing his wife’s shoulders and telling her that everything would be alright. But, Rose kept saying “I know we’ll have to sell the house and move into something smaller, and I am going to be blind Charlie. Blind.”
I could hear Charlie rubbing his wife’s shoulders and telling her that everything would be alright. But, Rose kept saying “I know we’ll have to sell the house and move into something smaller, and I am going to be blind Charlie. Blind.” Today, people are living longer than ever before so it’s important to be proactive and take responsibility for your health as you age.
Today, people are living longer than ever before so it’s important to be proactive and take responsibility for your health as you age. 
 Maintain a healthy weight. Being overweight increases your risk for diabetes. By exercising regularly, you can help keep your body healthy and prevent vision loss.
Maintain a healthy weight. Being overweight increases your risk for diabetes. By exercising regularly, you can help keep your body healthy and prevent vision loss.  Don’t smoke. Smoking increases your risk for age-related macular degeneration, cataract, and other eye diseases and conditions that can damage the optic nerve.
Don’t smoke. Smoking increases your risk for age-related macular degeneration, cataract, and other eye diseases and conditions that can damage the optic nerve. Wear protective eyewear when outdoors. Protecting your eyes from the sun’s ultraviolet rays when you are outdoors is vital for your eye health. Wearing sunglasses that block 99 to 100 percent of both UV-A and UV-B radiation.
Wear protective eyewear when outdoors. Protecting your eyes from the sun’s ultraviolet rays when you are outdoors is vital for your eye health. Wearing sunglasses that block 99 to 100 percent of both UV-A and UV-B radiation. Know your family history. Talk to your family members about their eye health history. It’s important to know if anyone has been diagnosed with a disease or condition since many are hereditary, such as glaucoma, macular degeneration, and diabetes . This will help determine if you are at higher risk for developing an eye disease or condition.
Know your family history. Talk to your family members about their eye health history. It’s important to know if anyone has been diagnosed with a disease or condition since many are hereditary, such as glaucoma, macular degeneration, and diabetes . This will help determine if you are at higher risk for developing an eye disease or condition. Consider a multivitamin. Vitamins C, E and the mineral zinc have been shown to promote eye health. Vitamins with Lutein and Zeaxanthin have been known to help patients with moderate to severe age-related macular degeneration.
Consider a multivitamin. Vitamins C, E and the mineral zinc have been shown to promote eye health. Vitamins with Lutein and Zeaxanthin have been known to help patients with moderate to severe age-related macular degeneration. Give your eyes a rest. If you spend a lot of time at the computer or focusing at any one distance, you sometimes forget to blink, resulting in dryness and eye fatigue. Every 20 minutes, look away about 20 feet in front of you for 20 seconds. This can help reduce eyestrain. Consider using a lubricant eye drop during long periods of intense eye use and rest your eyes for 5 minutes.
Give your eyes a rest. If you spend a lot of time at the computer or focusing at any one distance, you sometimes forget to blink, resulting in dryness and eye fatigue. Every 20 minutes, look away about 20 feet in front of you for 20 seconds. This can help reduce eyestrain. Consider using a lubricant eye drop during long periods of intense eye use and rest your eyes for 5 minutes.