 Taking care of your health is critical and you may have concerns related to eye health as a result of the COVID-19 pandemic. The offices of Ophthalmologists and Optometrists are resuming the delivery of comprehensive eye and vision care and implementing new protocols to provide care in a safe and healthy environment.
Taking care of your health is critical and you may have concerns related to eye health as a result of the COVID-19 pandemic. The offices of Ophthalmologists and Optometrists are resuming the delivery of comprehensive eye and vision care and implementing new protocols to provide care in a safe and healthy environment.
While changes vary from state-to-state as well as individual practice locations, patients should expect that their eye doctors, like all medical professionals, are adhering to federal, state and local health directives regarding infection prevention measures and implementing appropriate safety procedures to reduce the risk of COVID-19 transmission within the office. These not only include strict protocols for cleaning and sterilization, but measures to effectively manage patient flow and encourage physical distancing. Patients should expect screenings for symptoms of COVID-19 and taking patients’ temperature upon their arrival at the facility, limiting the number of guests allowed in waiting rooms and requiring everyone to wear a facemask and/or gloves before entering the office.
Prior to the appointment, you should be asked a series of questions such as whether you have been diagnosed with COVID-19, whether you have been exposed to anyone who has an active COVID infection, and whether you have any of the typical symptoms of a COVID-19 infection including fever, cough, shortness of breath, or some impairment of your sense of taste or smell. You may also be asked about recent travel history. If there is a concern that you may have COVID-19 infection, then the appointment may be rescheduled to a later date.
Once you get to the office, you will be interviewed again to see if you have any symptoms suggestive of COVID-19 infection. You may be asked to have your temperature taken with a non-contact thermometer and to wash your hands or scrub your hands with hand sanitizer before entering the office. You may be asked not to bring any family members or assistants with you.
Every patient (and anyone accompanying the patient) is required to wear a mask, and the mask must be worn properly, covering both the nose and mouth. The mask must be worn through the entire visit, and conversations with the doctor or staff will be limited. The tests that are used to monitor glaucoma may be performed with modified protocols to minimize the time you spend at the office.
How to Prepare for Your Eye Doctor Visit
- Don’t go if you’re feeling sick. If you wake up with a cough or a sore throat, it’s probably best to reschedule your appointment and call your primary physician. Your routine eye exam can wait. Don’t be surprised if someone takes your temperature upon arrival to ensure safety for everyone.
- Fill out forms in advance. If possible, fill out your intake forms online before your appointment. This will limit your face-to-face contact and your overall time within the office. Any additional information that’s requested by your doctor can also be done over the phone.
- Follow social distancing guidelines. There may be new procedures in place to help with social distancing, from markers on the ground indicating where to stand, to a limited number of people allowed in certain areas. Depending upon the office location, you may need to call from your car to check in. Every office is different, so be sure to check with your doctor’s office about their requirements.
- Go alone to your appointment. Most offices are only allowing the patient to enter the office, with the exception of those who require a caregiver or a guardian to attend the appointment with them. This limits the amount of people going in and out of the office, and helps maintain a more sterile, clean environment.
- Wear a mask to your appointment. Depending on your state, a mask may either be mandated or highly recommended when you are in public places. The Centers for Disease Control and Prevention highly advises people to wear a mask covering their nose and their mouth in order to help stop the spread of COVID-19.
As your eye care doctors begin reopening and operations proceed under a “new normal,” your ophthalmologist and/or optometrist are working to ensure the continued safe delivery of essential eye care during the COVID-19 pandemic.
To know exactly what to expect during your appointment, call your doctor’s office to find out how to best prepare for your visit.



 Tom Sullivan
Tom Sullivan




 Step 1: Light passes through a thin layer of moisture
Step 1: Light passes through a thin layer of moisture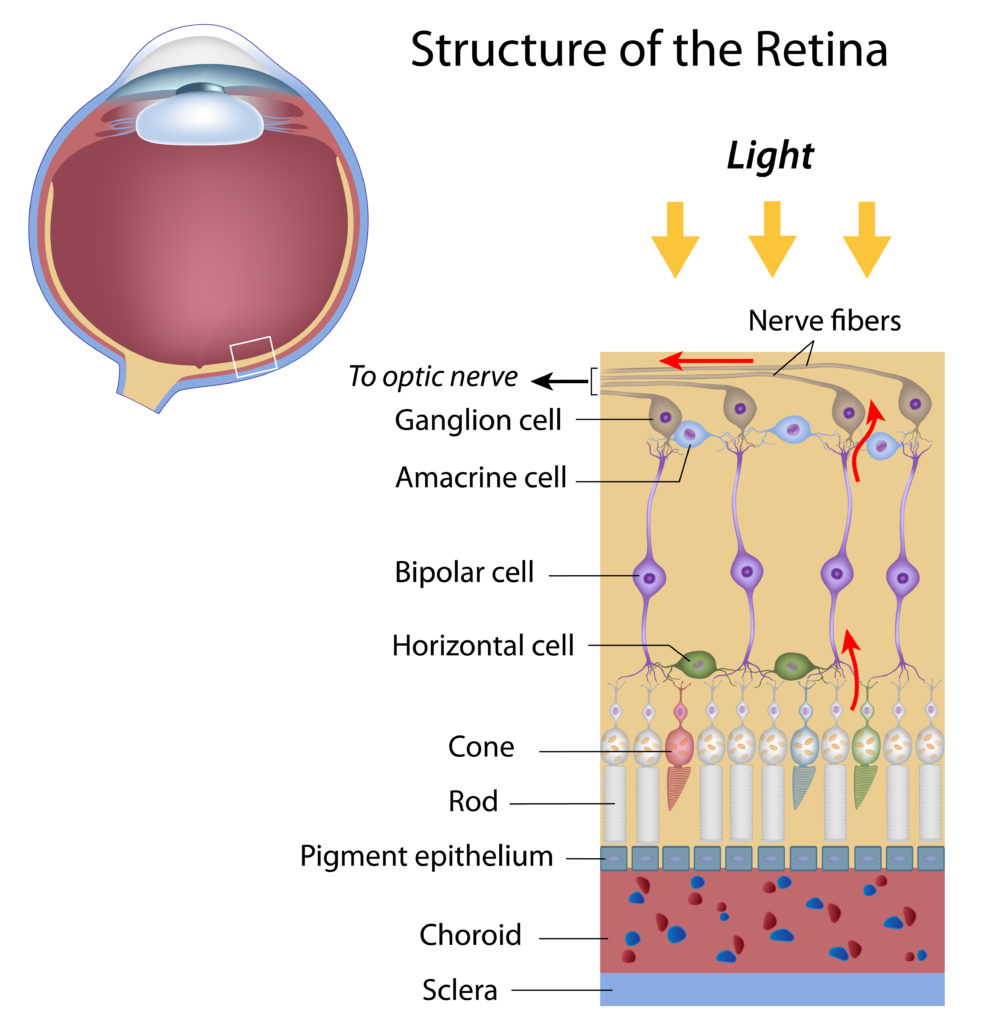
 National Glaucoma Awareness Month reminds all of us to get regular eye exams and show support for those suffering from this condition.
National Glaucoma Awareness Month reminds all of us to get regular eye exams and show support for those suffering from this condition. 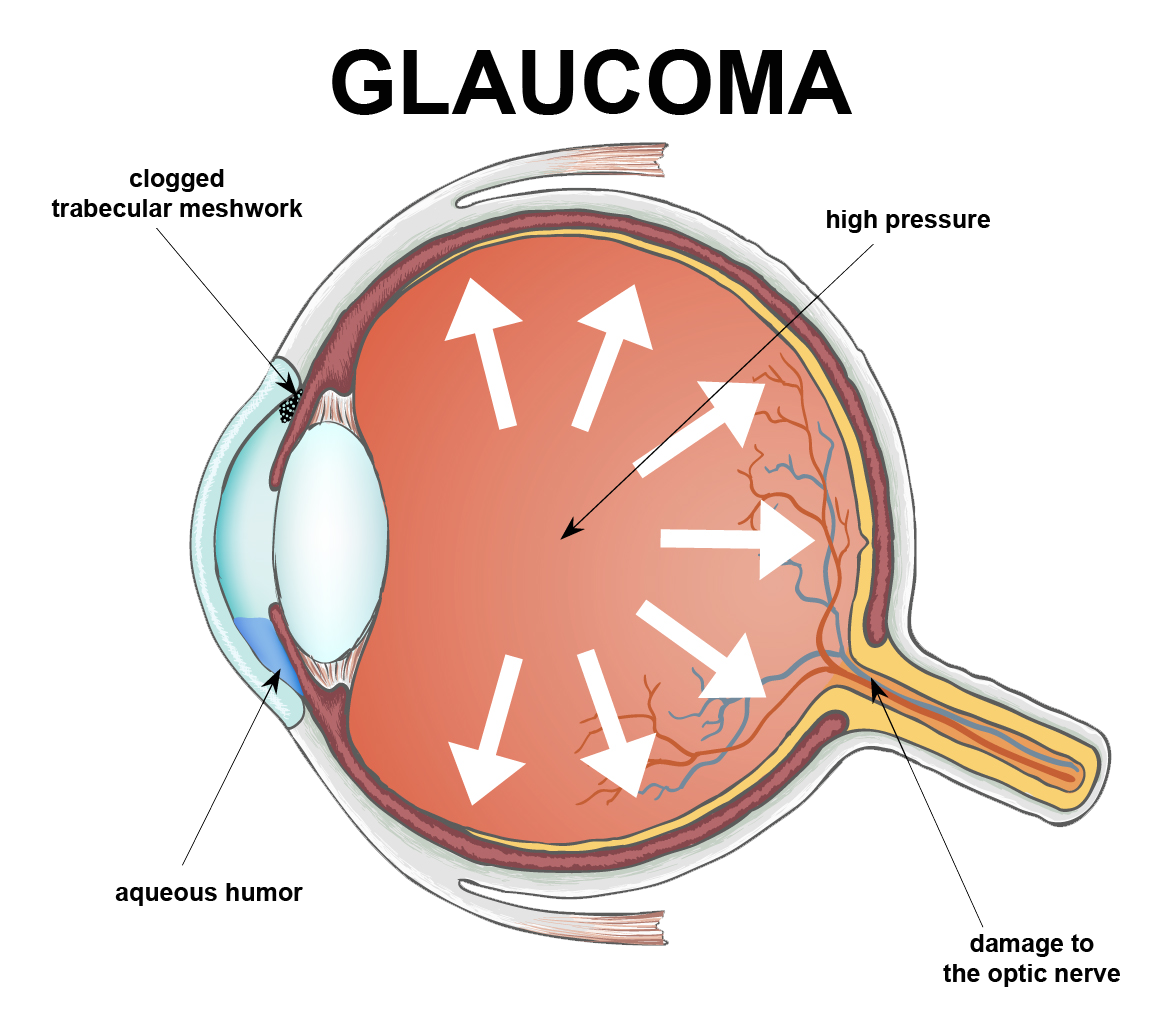


 Thanksgiving is almost here; a meal that nourishes the family bonds and traditions. It’s the one time of the year where you can guarantee your eyes will be bigger than your stomach.
Thanksgiving is almost here; a meal that nourishes the family bonds and traditions. It’s the one time of the year where you can guarantee your eyes will be bigger than your stomach.