Harsh weather conditions can reduce the natural moisture in your eyes and the irritation usually results in a burning or itching sensation that often leads to rubbing or scratching your eyes which can worsen the symptoms. Sometimes it feels like there is a foreign object in your eye and for some, dry eyes can even cause excessive tearing, as your eyes try to overcompensate for their lack of protective tears. Prolonged, untreated dry eyes can lead to blurred vision as well. Between the harsh winter winds outside and the dry heat radiating inside, our eyes are very quickly irritated and dried in the winter months. The result is itchy, dry eyes that may cause pain, blurred vision, a burning sensation, or even watery vision as our eyes try to compensate for the dryness.
Harsh weather conditions can reduce the natural moisture in your eyes and the irritation usually results in a burning or itching sensation that often leads to rubbing or scratching your eyes which can worsen the symptoms. Sometimes it feels like there is a foreign object in your eye and for some, dry eyes can even cause excessive tearing, as your eyes try to overcompensate for their lack of protective tears. Prolonged, untreated dry eyes can lead to blurred vision as well. Between the harsh winter winds outside and the dry heat radiating inside, our eyes are very quickly irritated and dried in the winter months. The result is itchy, dry eyes that may cause pain, blurred vision, a burning sensation, or even watery vision as our eyes try to compensate for the dryness.
What Are The Symptoms?
- Uncomfortable, stingy, burning or scratchy feeling.
- Stringy mucus in or around your eyes
- Increased eye irritation from smoke or wind
- Eye fatigue
- Sensitivity to light
- Eye redness
- A sensation of having something in your eyes
- Difficulty wearing contact lenses
- Periods of excessive tearing
- Blurred vision, often worsening at the end of the day or after focusing for a prolonged period
10 TIPS TO KEEP YOUR EYES COMFORTABLE DURING THE WINTER MONTHS
Whatever the symptoms, dry eyes can cause significant discomfort during the long winters and relief can seriously improve your quality of life.
- To keep eyes moist, apply artificial tears/eye drops a few times a day. If you have chronic dry eyes, speak to your eye doctor about the best product for your condition.
- Drink a lot of fluids – keeping your body hydrated will also help maintain the moisture in your eyes.
- If you spend a lot of time indoors in heated environments, use a humidifier to add some moisture back into the air.
- Try to situate yourself away from sources of heat, especially if they are blowing. While a nice cozy fire can add to the perfect winter evening, make sure to keep your distance so dry eyes don’t ruin it.
- Staring at a computer or digital device for extended amounts of time can further dry out your eyes. If you spend a lot of time staring at the screen, make sure you blink often and practice the 20/20/20 rule – every 20 minutes, look 20 feet away for 20 seconds. Use artificial tears often to lubricate eyes during long periods of using your eyes.
- Avoid air blowing in your eyes. Don’t direct hair dryers, car heaters, air conditioners or fans toward your eyes. In your car, direct heat to floor vents and away from your eyes once your windshield is defrosted.
- Stop smoking and avoid smoky environments.
- Don’t rub your eyes! This will only increase irritation and can also lead to infections if your hands are not clean.
- Give your eyes a break and break out your glasses. If your contact lenses are causing further irritation, take a break and wear your glasses for a few hours or days. Also talk to your optometrist about switching to contacts that are better for dry eyes.
- Protect your eyes. If you know you are going to be venturing into harsh weather conditions, such as extreme cold or wind, make sure you wear protection. Try large, 100% UV protective eyeglasses and a hat with a visor to keep the wind and particles from getting near your eyes. If you are a winter sports enthusiast, make sure you wear well-fitted ski goggles.
If you find that after following these tips you continue to suffer, contact your eye doctor.


 I can only imagine my wife’s beautiful face. Oh sure, I’ve touched it and kissed it many times. I’ve felt the lines with the tips of my fingers, tracing our lives together, and I’ve heard her smile. I understand that’s not really seeing it. It’s not seeing her eyes as they sparkle with something funny I said; or, when she looks at me with love reserved only for those who are truly in love.
I can only imagine my wife’s beautiful face. Oh sure, I’ve touched it and kissed it many times. I’ve felt the lines with the tips of my fingers, tracing our lives together, and I’ve heard her smile. I understand that’s not really seeing it. It’s not seeing her eyes as they sparkle with something funny I said; or, when she looks at me with love reserved only for those who are truly in love.
 Tom Sullivan
Tom Sullivan Costume Contact Lenses such as cat eyes or zombie may make your Halloween costume a bit more frightful although wearing those lenses without a prescription can be more terrifying, as it could result in vision loss or even blindness.
Costume Contact Lenses such as cat eyes or zombie may make your Halloween costume a bit more frightful although wearing those lenses without a prescription can be more terrifying, as it could result in vision loss or even blindness.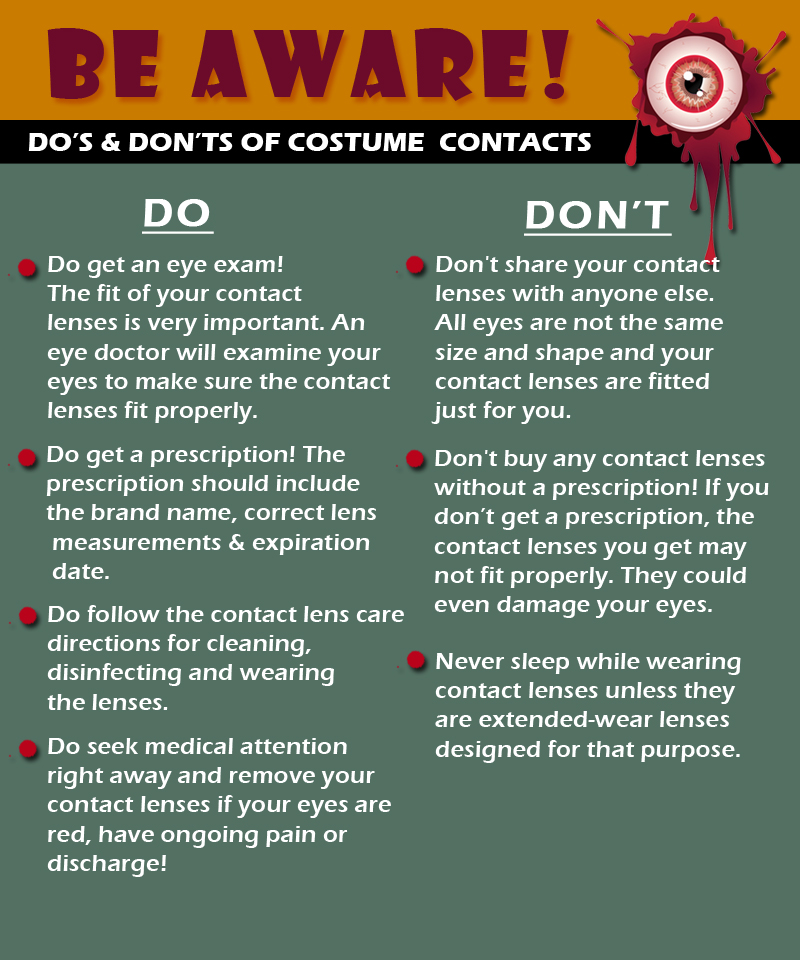
 Today, people are living longer than ever before so it’s important to be proactive and take responsibility for your health as you age.
Today, people are living longer than ever before so it’s important to be proactive and take responsibility for your health as you age. 
 Maintain a healthy weight. Being overweight increases your risk for diabetes. By exercising regularly, you can help keep your body healthy and prevent vision loss.
Maintain a healthy weight. Being overweight increases your risk for diabetes. By exercising regularly, you can help keep your body healthy and prevent vision loss.  Don’t smoke. Smoking increases your risk for age-related macular degeneration, cataract, and other eye diseases and conditions that can damage the optic nerve.
Don’t smoke. Smoking increases your risk for age-related macular degeneration, cataract, and other eye diseases and conditions that can damage the optic nerve. Wear protective eyewear when outdoors. Protecting your eyes from the sun’s ultraviolet rays when you are outdoors is vital for your eye health. Wearing sunglasses that block 99 to 100 percent of both UV-A and UV-B radiation.
Wear protective eyewear when outdoors. Protecting your eyes from the sun’s ultraviolet rays when you are outdoors is vital for your eye health. Wearing sunglasses that block 99 to 100 percent of both UV-A and UV-B radiation.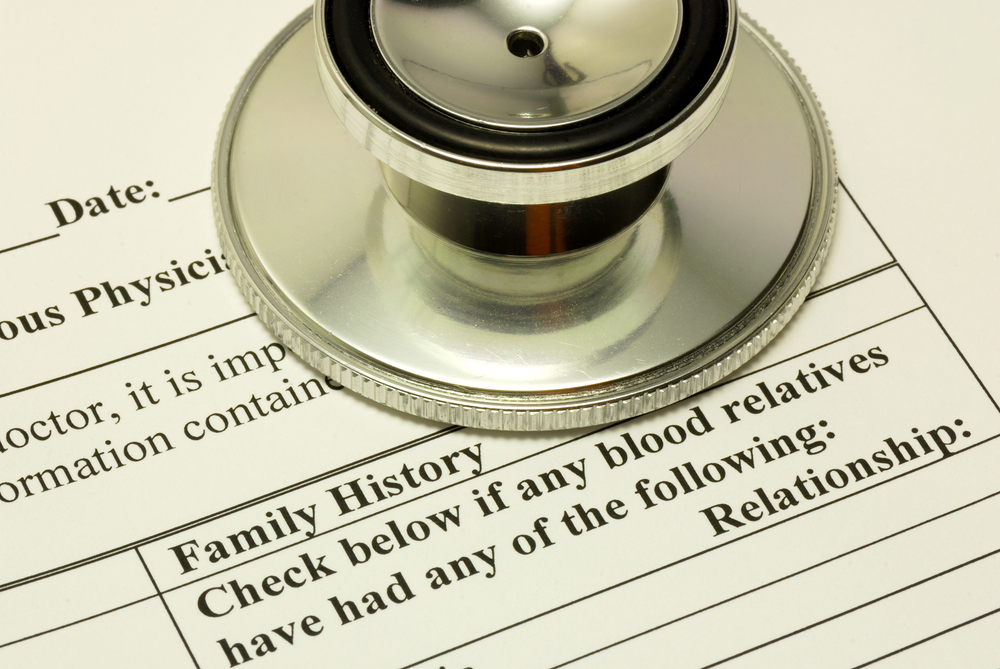 Know your family history. Talk to your family members about their eye health history. It’s important to know if anyone has been diagnosed with a disease or condition since many are hereditary, such as glaucoma, macular degeneration, and diabetes . This will help determine if you are at higher risk for developing an eye disease or condition.
Know your family history. Talk to your family members about their eye health history. It’s important to know if anyone has been diagnosed with a disease or condition since many are hereditary, such as glaucoma, macular degeneration, and diabetes . This will help determine if you are at higher risk for developing an eye disease or condition. Consider a multivitamin. Vitamins C, E and the mineral zinc have been shown to promote eye health. Vitamins with Lutein and Zeaxanthin have been known to help patients with moderate to severe age-related macular degeneration.
Consider a multivitamin. Vitamins C, E and the mineral zinc have been shown to promote eye health. Vitamins with Lutein and Zeaxanthin have been known to help patients with moderate to severe age-related macular degeneration. Give your eyes a rest. If you spend a lot of time at the computer or focusing at any one distance, you sometimes forget to blink, resulting in dryness and eye fatigue. Every 20 minutes, look away about 20 feet in front of you for 20 seconds. This can help reduce eyestrain. Consider using a lubricant eye drop during long periods of intense eye use and rest your eyes for 5 minutes.
Give your eyes a rest. If you spend a lot of time at the computer or focusing at any one distance, you sometimes forget to blink, resulting in dryness and eye fatigue. Every 20 minutes, look away about 20 feet in front of you for 20 seconds. This can help reduce eyestrain. Consider using a lubricant eye drop during long periods of intense eye use and rest your eyes for 5 minutes.


 Summer time is officially here and everyone enjoys a dip in a nice, cool pool during the summer months. While swimming is a great form of exercise and a relaxing way to cool down, the water can be hard on your eyes.
Summer time is officially here and everyone enjoys a dip in a nice, cool pool during the summer months. While swimming is a great form of exercise and a relaxing way to cool down, the water can be hard on your eyes. Wear Goggles – Wear a pair of swim goggles every time you swim. Goggles keep pool chemicals out of your eyes.
Wear Goggles – Wear a pair of swim goggles every time you swim. Goggles keep pool chemicals out of your eyes. Wash Your Eyes – Immediately after swimming, splash your closed eyes with fresh tap water. This washes chlorine and other chemicals off your eyelids and eyelashes.
Wash Your Eyes – Immediately after swimming, splash your closed eyes with fresh tap water. This washes chlorine and other chemicals off your eyelids and eyelashes. Use Eye Drops – Use over-the-counter lubricating eye drops before and after swimming to keep the tear film balanced and eyes comfortable.
Use Eye Drops – Use over-the-counter lubricating eye drops before and after swimming to keep the tear film balanced and eyes comfortable. Stay Hydrated – Don’t forget to drink plenty of water. Staying well hydrated is an important part of keeping your eyes moist and comfortable.
Stay Hydrated – Don’t forget to drink plenty of water. Staying well hydrated is an important part of keeping your eyes moist and comfortable.
 Most problems associated with contact lenses cause minor irritation, but serious eye infections from poor lens hygiene can be extremely painful and may lead to permanent vision loss. About 80 to 90 percent of contact lens-related eye infections are bacterial. A type of infection you can get is called pseudomonas aeruginosa, a fast-growing bacterial infection that can lead to a hole in your cornea. Unfortunately, patients who get this infection have a high chance of permanent scarring and vision loss. Beyond bacteria, fungal infections are also potential threats to your vision.
Most problems associated with contact lenses cause minor irritation, but serious eye infections from poor lens hygiene can be extremely painful and may lead to permanent vision loss. About 80 to 90 percent of contact lens-related eye infections are bacterial. A type of infection you can get is called pseudomonas aeruginosa, a fast-growing bacterial infection that can lead to a hole in your cornea. Unfortunately, patients who get this infection have a high chance of permanent scarring and vision loss. Beyond bacteria, fungal infections are also potential threats to your vision.