If you need eyeglasses, it is because you were diagnosed with a refractive error during your eye exam. This means your eyes have trouble focusing and images can appear blurry. Types of refractive errors include being near-sighted (myopia), far-sighted (presbyopia) or having an astigmatism (your cornea is an irregular shape).
 Understanding What 20/20 Vision Means
Understanding What 20/20 Vision Means
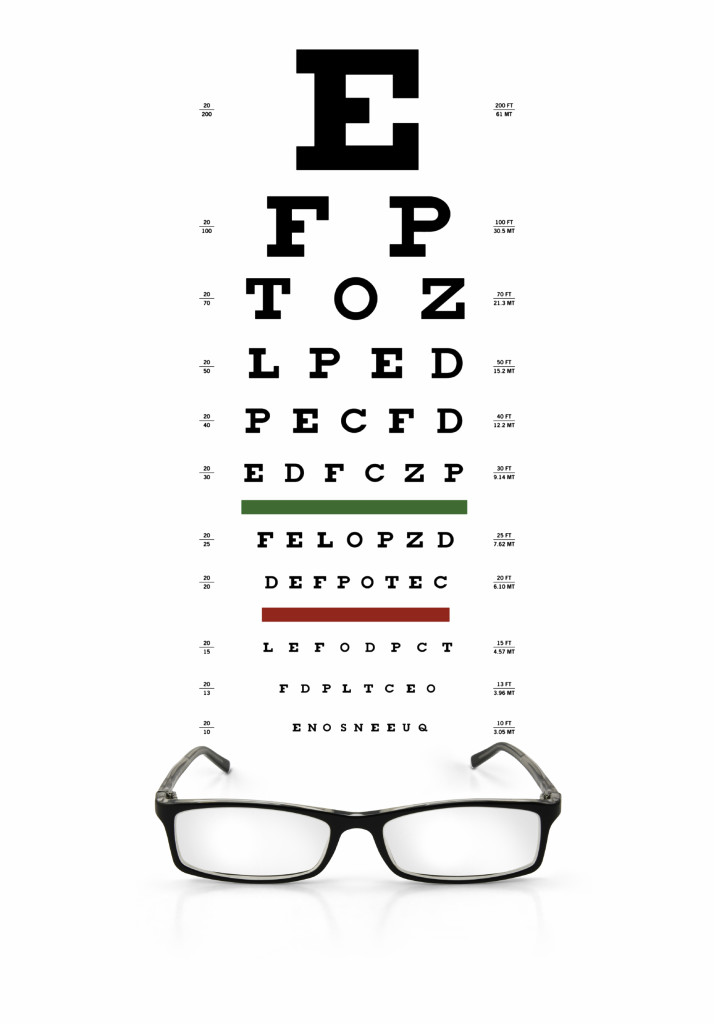
The number is based on you standing a distance of 20 feet in front of a standard eye chart to test your visual acuity. If during an eye test you can read the big E at the top of the eye chart, but none of the letters below that, your vision is considered 20/200. That means you can read a letter at 20 feet that people with “normal” vision can read at 200 feet, meaning you have very poor distance visual acuity. If you can read the seventh line from the top of most charts, your vision is 20/20. Any line below that would be 20/15 or below and indicates that you have exceptional visual acuity. Each eye is tested separately.
Understanding Your Eyeglass Prescription
The prescription you receive may be a form with headings that are filled in, or it may just be written out. In any case, it is written in a specific order, with the results for each eye listed separately.
OD is an abbreviation for oculus dexter, meaning right eye, while OS is oculus sinister, meaning left eye. If both eyes are being referred to the abbreviation you will see is OU (oculus uterque) meaning both eyes.
The next term on your prescription is Sphere (SPH) and is are measured in diopters (D). This number tells you how strong your lenses need to be to correct your vision. If this number has a minus sign (–), you are nearsighted; if the number has a plus sign (+) or is not preceded by any sign, you are farsighted.
Next may be cylinder (CYL), an indicator of the lens power if you have an astigmatism. The number for the CYL has the same format as the SPH, a minus sign (for the correction of nearsighted astigmatism) or a plus sign (for the correction of farsighted astigmatism). If there is no number given you either have no astigmatism, or your astigmatism is so slight that it is not really necessary to correct it.
If you do have a CYL number you will also have an axis number, based on a protractor scale that tells you where on the eye the astigmatism is found. For example,
SPH –2.50 CYL +5.00 Axis 40 means you have a nearsightedness of -2.50 diopters with an astigmatism of +5.00 along the 40 degree axis.
If you are getting bifocals or progressive lenses, there is another number called an “Add.” This number is the amount of additional correction your eyes need to focus at close distance and will always be a positive number, whether or not the + sign is there.
Needless to say, eyeglasses can be expensive, but understanding a prescription should help you understand why. The stronger the lens the more expensive it is and then with each adjustment, the cost also increases. Also, don’t forget that anti-glare or UV protective coatings add to the costs, but most people feel it is well worth it. Eye glasses are an investment in your safety, job, independence and letting you enjoy leisure-time activities you enjoy.



 Save Your Vision Month is here.
Save Your Vision Month is here.


 Harsh weather conditions can reduce the natural moisture in your eyes and the irritation usually results in a burning or itching sensation that often leads to rubbing or scratching your eyes which can worsen the symptoms. Sometimes it feels like there is a foreign object in your eye and for some, dry eyes can even cause excessive tearing, as your eyes try to overcompensate for their lack of protective tears. Prolonged, untreated dry eyes can lead to blurred vision as well. Between the harsh winter winds outside and the dry heat radiating inside, our eyes are very quickly irritated and dried in the winter months. The result is itchy, dry eyes that may cause pain, blurred vision, a burning sensation, or even watery vision as our eyes try to compensate for the dryness.
Harsh weather conditions can reduce the natural moisture in your eyes and the irritation usually results in a burning or itching sensation that often leads to rubbing or scratching your eyes which can worsen the symptoms. Sometimes it feels like there is a foreign object in your eye and for some, dry eyes can even cause excessive tearing, as your eyes try to overcompensate for their lack of protective tears. Prolonged, untreated dry eyes can lead to blurred vision as well. Between the harsh winter winds outside and the dry heat radiating inside, our eyes are very quickly irritated and dried in the winter months. The result is itchy, dry eyes that may cause pain, blurred vision, a burning sensation, or even watery vision as our eyes try to compensate for the dryness.
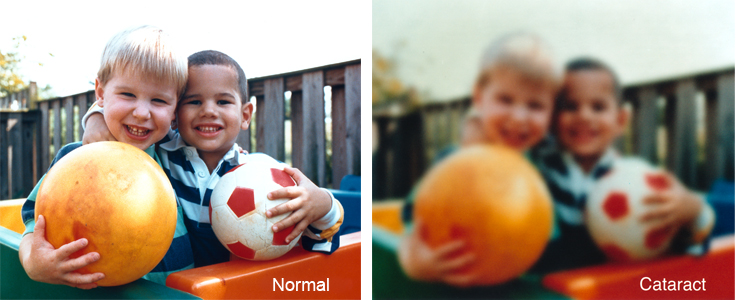
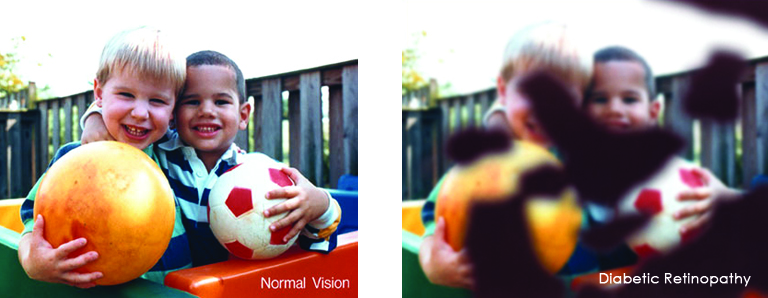
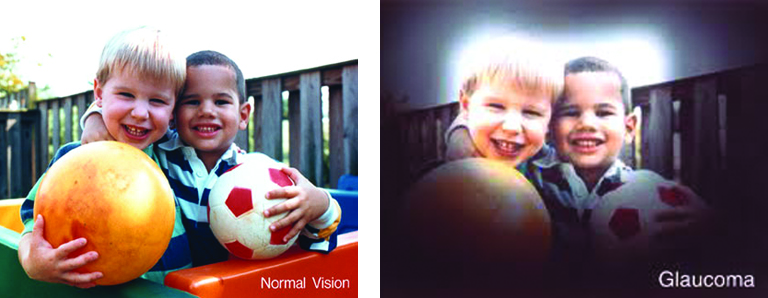
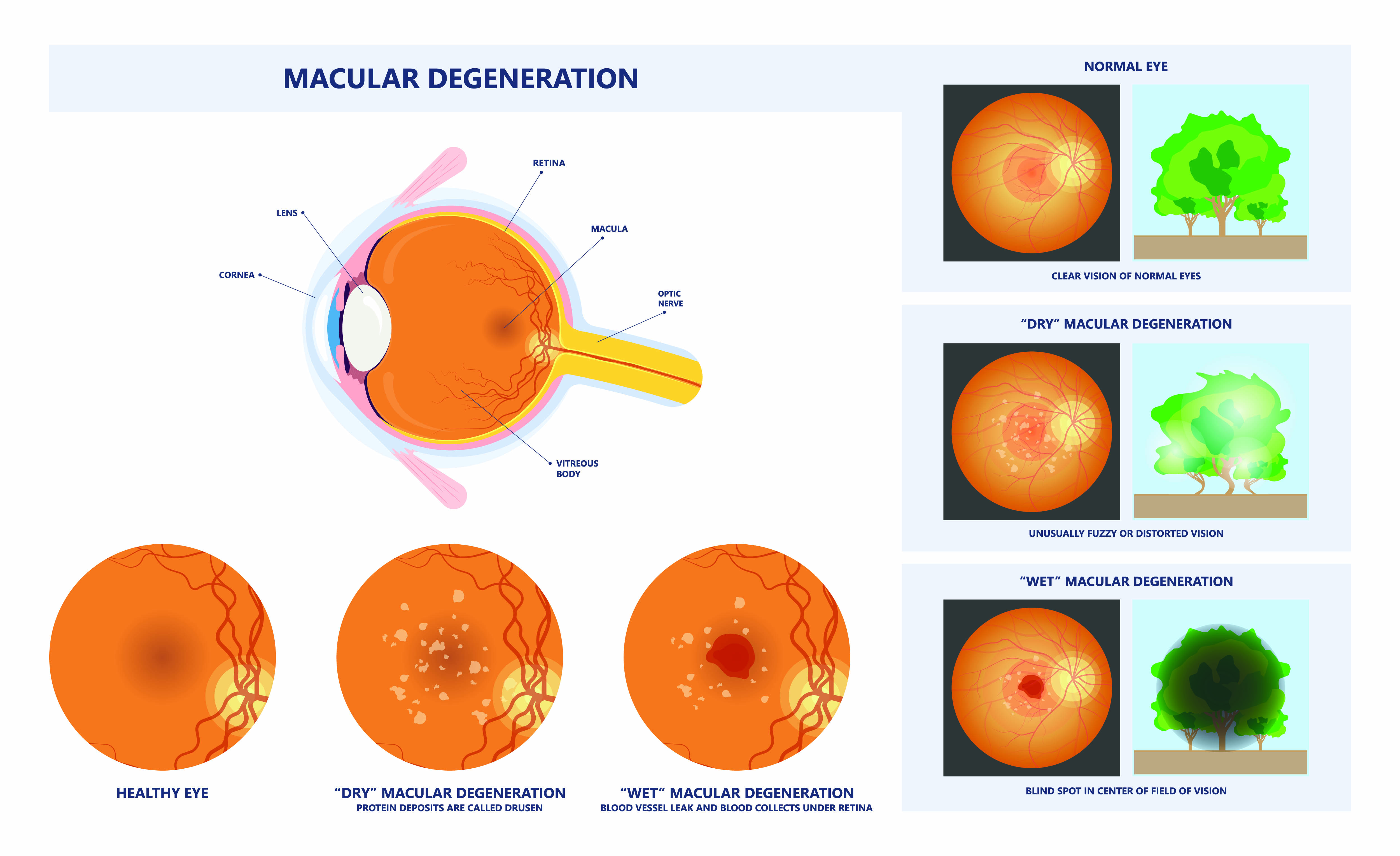
 Most people have eye problems at one time or another. Some are minor and will go away on their own, or are easy to treat at home. Others need a specialist’s care. Some eye issues come with age while others may be a serious condition.
Most people have eye problems at one time or another. Some are minor and will go away on their own, or are easy to treat at home. Others need a specialist’s care. Some eye issues come with age while others may be a serious condition. Dry eye is a common condition that occurs when your tears aren’t able to provide adequate lubrication for your eyes. Tears can be inadequate for many reasons. For example, dry eyes may occur if you don’t produce enough tears or if you produce poor-quality tears. Dry eyes can also feel very uncomfortable.
Dry eye is a common condition that occurs when your tears aren’t able to provide adequate lubrication for your eyes. Tears can be inadequate for many reasons. For example, dry eyes may occur if you don’t produce enough tears or if you produce poor-quality tears. Dry eyes can also feel very uncomfortable.