On Robert Louis Stevenson’s first visit to the Monterey Peninsula of California he was overwhelmed by its vistas and beauty. He wrote to friends that what he had observed was the perfect confluence of land and sea.
At this writing I am vacationing with my family in a home that sits on the very same beach that allowed Stevenson the awesome privilege of observing the horseshoe of Carmel Bay with Point Lobos rising out of the morning fog in the distance.
 My daughter Blythe holds binoculars up to her eyes and watches a family of otters play joyously in and out of the kelp. They’re not alone. My wife Patty is laughing as she checks out a group of sea lions in their own game of tag, and the sound of their barking makes me smile. Later that day I’ll hear the appreciative ooh and aah of my family as they watch the sun knife its way into the ocean with its promise to rise again in the morning.
My daughter Blythe holds binoculars up to her eyes and watches a family of otters play joyously in and out of the kelp. They’re not alone. My wife Patty is laughing as she checks out a group of sea lions in their own game of tag, and the sound of their barking makes me smile. Later that day I’ll hear the appreciative ooh and aah of my family as they watch the sun knife its way into the ocean with its promise to rise again in the morning.
We’ve had our dinner and my son Tom tells me about the stars that dot the sky. “Dad” he says, “I wish you could see them.” There’s the constant North Star that always serves sailors on a dark night along with the supporting cast of constellations lead by Scorpio. I can hear the love in Tom’s voice when he again says, “I’d give anything if you could just look at all this beauty Dad.”
I must confess that I’d like to wish on those stars and maybe have my vision for oh-let’s say-one day. I think I’d start with the faces of the people I love and then move on taking in nature and all its glory. It would mean so much if I could see the innocence of a beautiful child’s smiling face. If I am lucky, there might be a rain shower followed by all the colors of a rainbow.
I am not complaining, I’ve enjoyed a world of four senses that most of you never take the time to truly appreciate. On this vacation I am on sensory overload with smell, taste, sound, and touch. So again, let me reiterate that I am not complaining. What I’ve come to understand is that sight is the dominant sense. It offers all of you a perspective on the world that I can only imagine.
So, the old chestnut really is true. Beauty is in the eyes of the beholder and at the Discovery Eye Foundation, our researchers work tirelessly every day to ensure that you and those you love have the chance to consider and appreciate all of the beauty that surrounds us.
With your help our efforts will continue to preserve vision and eliminate blindness for people around the world.
Donate today to help support the Discovery Eye Foundation!
 Tom Sullivan
Tom Sullivan
DEF’s Ambassador of Vision
sullivanvision.com










 Some studies have found that fish oil can reverse dry eye, including dry eye caused by spending too much time on a computer.
Some studies have found that fish oil can reverse dry eye, including dry eye caused by spending too much time on a computer.
 Citrus fruits are rich in vitamin C. Just like vitamin E, vitamin C is an antioxidant that is recommended to fight age-related eye damage.
Citrus fruits are rich in vitamin C. Just like vitamin E, vitamin C is an antioxidant that is recommended to fight age-related eye damage.

 Beef is rich in zinc, which has been linked to better long-term eye health. Zinc can help delay age-related sight loss and macular degeneration.
Beef is rich in zinc, which has been linked to better long-term eye health. Zinc can help delay age-related sight loss and macular degeneration.
 It may come as no surprise that a fluid essential to life is also vital to eye health.
It may come as no surprise that a fluid essential to life is also vital to eye health.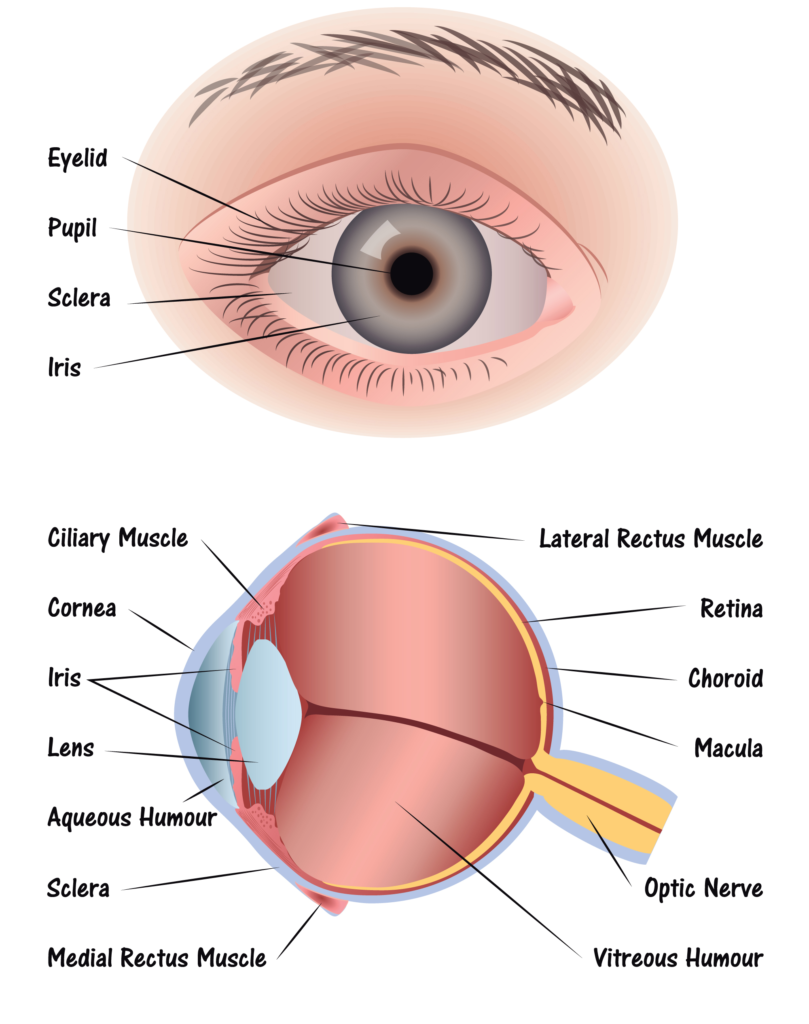 Step 1: Light passes through a thin layer of moisture
Step 1: Light passes through a thin layer of moisture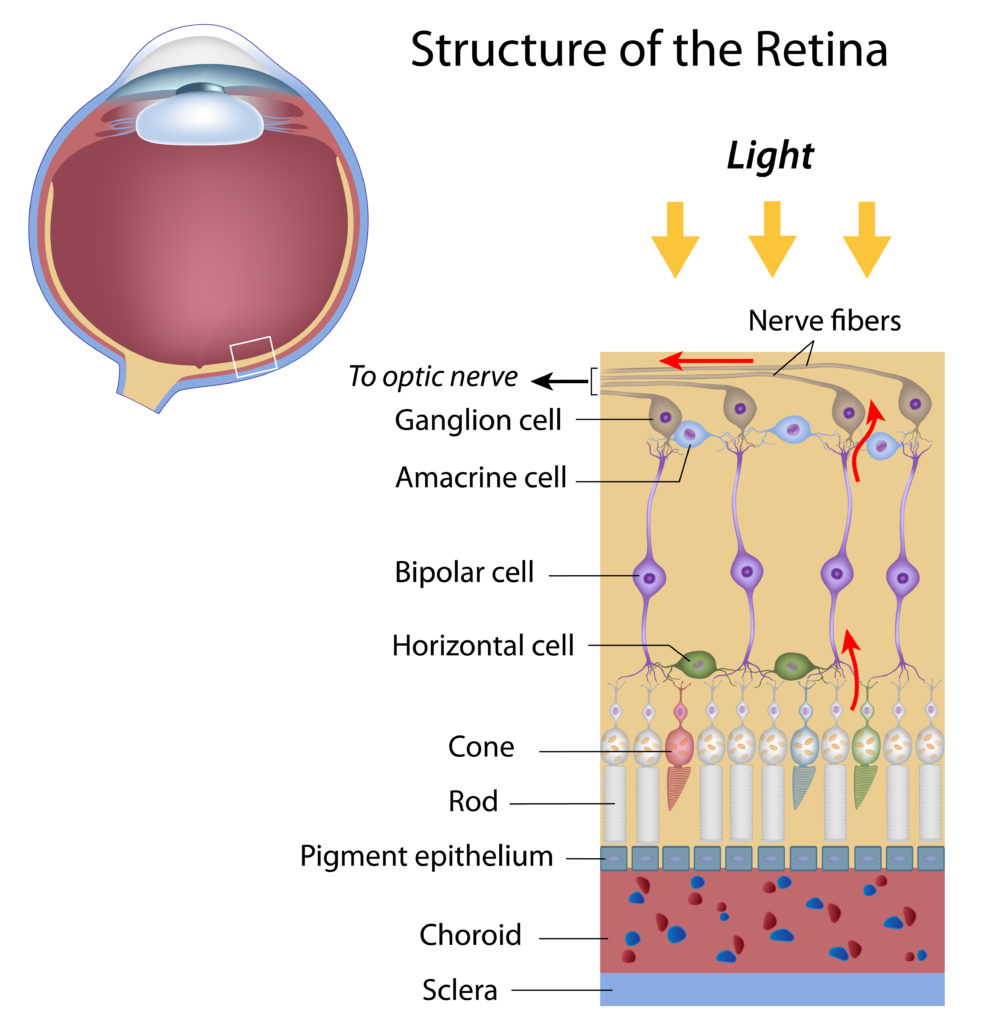
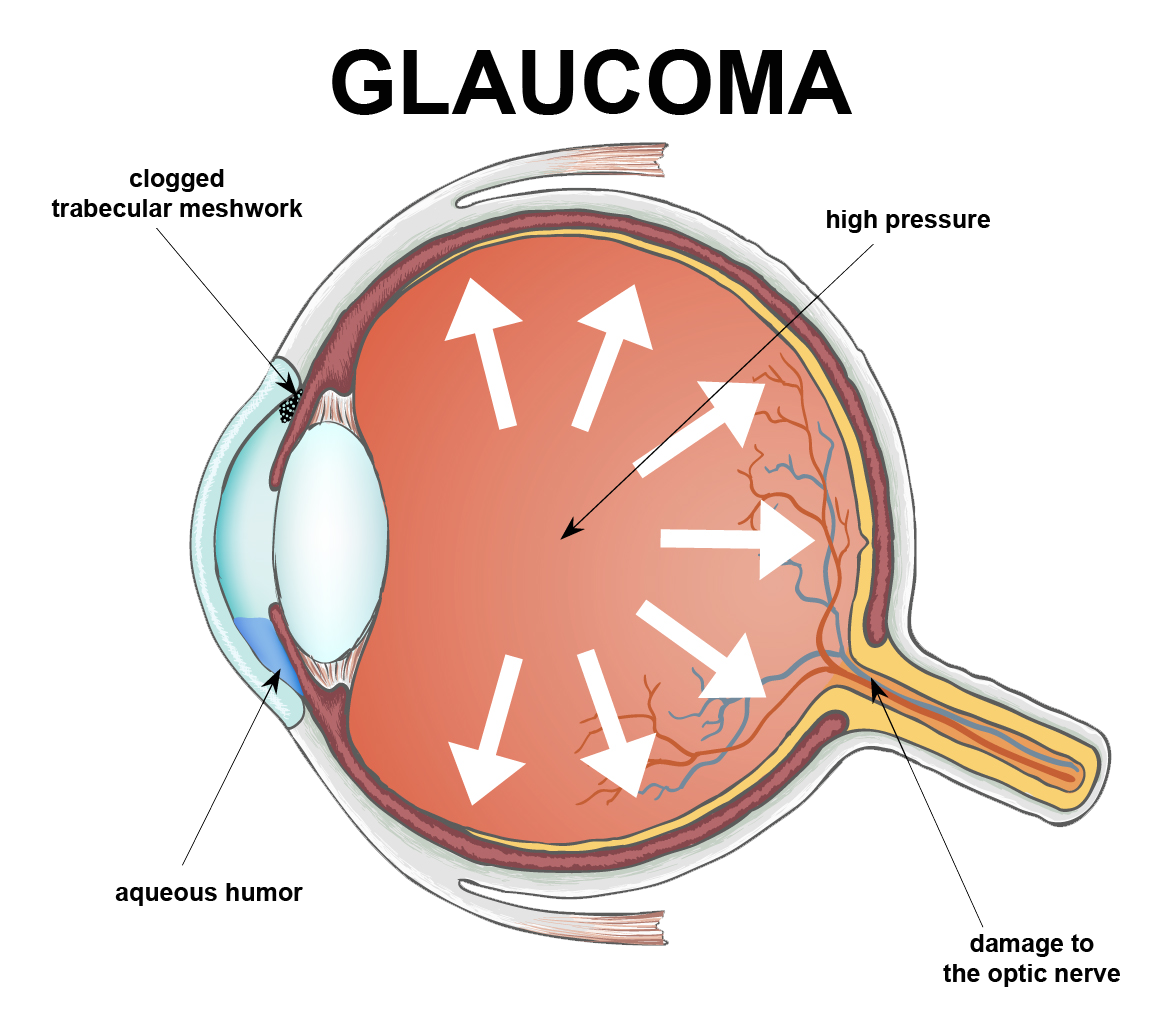
 National Glaucoma Awareness Month reminds all of us to get regular eye exams and show support for those suffering from this condition.
National Glaucoma Awareness Month reminds all of us to get regular eye exams and show support for those suffering from this condition.